-
丙戊酸钠(valproate acid,VPA)是临床上常用的广谱抗癫痫药,对各种类型癫痫均有治疗作用,且广泛用于其他神经系统疾病[1-2]。研究显示,长期使用VPA存在潜在的不良反应,临床上常见的不良反应主要有胰腺炎、致畸性和肝毒性,其中最严重的不良反应就是肝毒性,严重时甚至可发生急性肝坏死[3-4]。因此,深入研究VPA肝毒性的发病机制,对于预防VPA毒副作用和促进临床安全用药具有重要指导意义。
VPA在体内的代谢受多种因素影响,治疗窗范围窄,个体差异大,有效治疗血药浓度为50~100 μg/ml,超过100 μg/ml易产生不良反应,因此需要进行血药浓度监测[5-6]。VPA的毒副作用与其血药浓度相关,及时监测血药浓度可有效控制癫痫发作和减少不良反应发生。研究显示,VPA的肝毒性与其体内代谢特征相关,VPA及其代谢产物所诱导的线粒体功能障碍与肝毒性相关[7-9]。已有研究证明,VPA的不饱和代谢产物2-丙基-4-五烯酸(2-propyl-4-pentenoic acid,4-ene-VPA)能通过抑制线粒体脂肪酸的β氧化,还能通过各种代谢途径与谷胱甘肽反应使其大量消耗降低机体的抗氧化能力进而产生肝毒性。但是,少见有3-羟基丙戊酸(3-hydroxy valproic acid,3-OH-VPA)和5-羟基丙戊酸(5-hydroxy valproic acid,5-OH-VPA)与肝毒性相关的文献报道。本课题组前期对VPA及其代谢产物的体外肝毒性研究中发现,VPA及3个代谢产物对体外人正常肝细胞增殖具有一定抑制作用,且表现为时间依赖性和浓度依赖性[9]。本研究首次将VPA及其3个代谢产物血药浓度对肝毒性的诊断进行分析和比较,将VPA的3个代谢产物作为生物标志物用于临床肝损毒性诊断,为临床安全给药提供合理依据。
HTML
-
自2016年4月至2018年3月,收集海军军医大学附属长征医院临床药理实验室服用VPA治疗的癫痫患者血样,共收集肝功能正常癫痫患者血样205例,肝功能异常癫痫患者血样123例。入选标准:仅为癫痫患者无其他并发症,单用VPA治疗癫痫,取血时间点达稳态血药浓度,无联合用药,服药前后均做过肝功能检查者。排除标准:有其他并发症、服药前肝或肾功能异常、与其他药物联合使用患者。
-
安捷伦1200高效液相色谱串联安捷伦6410 A质谱仪(美国安捷伦公司),丙戊酸钠(VPA,批号:FLA3C,纯度:98%,东京化工有限公司),2-丙基-4-五烯酸(4-ene-VPA,批号:3-XAL-91-4,纯度98%)、3-羟基丙戊酸(3-OH-VPA,批号:1-TVP-92-13)、3-羟基丙戊酸(5-OH-VPA,批号:1-TVP-149-5)均购自多伦多研究化学品公司,苯甲酸(批号:TS0911CA14,纯度98%,上海源叶生物科技有限公司),甲醇、甲酸、醋酸铵均为进口色谱级试剂(德国Merck公司)。
-
本研究采用SPSS 17.0统计学软件进行数据处理,计量数据用(
$\bar x$ ± s)表示,采用单因素方差和t检验分析,以P < 0.05差异有统计学意义。
1.1. 样本来源
1.2. 仪器与试剂
1.3. 统计学方法
-
收集123例肝功能异常(谷丙转氨酶ALT>50)癫痫患者血样为实验组,男性96例,女性27例;205例肝功能正常癫痫患者血样为对照组,男性127例,女性78例。口服丙戊酸钠缓释片(德巴金),首次服药2周,调整剂量后1周,在患者血药浓度达稳态后,取清晨空腹静脉血2~3 ml,经3 000 r/min离心10 min,取血清监测血药浓度。
-
采用本课题组前期建立的LC-MS/MS测定VPA和其3个代谢产物3-OH-VPA、4-ene-VPA和5-OH-VPA的方法[10]。检测两组癫痫患者血样中的VPA及其代谢产物血药浓度。其中,VPA及其3个代谢产物标准曲线的线性范围分别为VPA:2~150 μg/ml;4-ene-VPA: 50~5 000 ng/ml;3-OH-VPA及5-OH-VPA:50~1 000 ng/ml。
2.1. 标本采集
2.2. 血药浓度的测定
-
将肝功能正常组与肝功能异常组患者的VPA及其3个代谢产物血药浓度分析比较,结果显示,肝功能异常组平均血药浓度比肝功能正常组高,且差异有统计学意义(P<0.05),提示肝毒性不仅与VPA血药浓度有关,且与代谢产物血药浓度也有关系,结果见表1。
组别 VPA(μg/ml) 4-ene-VPA(ng/ml) 3-OH-VPA(ng/ml) 5-OH-VPA(ng/ml) 肝功能正常组(n=205) 62.44 ± 31.24 3 229.34 ± 1 704.30 597.85 ± 396.13 446.01 ± 403.15 肝功能异常组(n=123) 83.50 ± 31.57** 4 306.01 ± 1 811.00** 740.43 ± 609.33* 795.14 ± 557.11** *P<0.05,**P<0.01,与肝功能正常组比较。 -
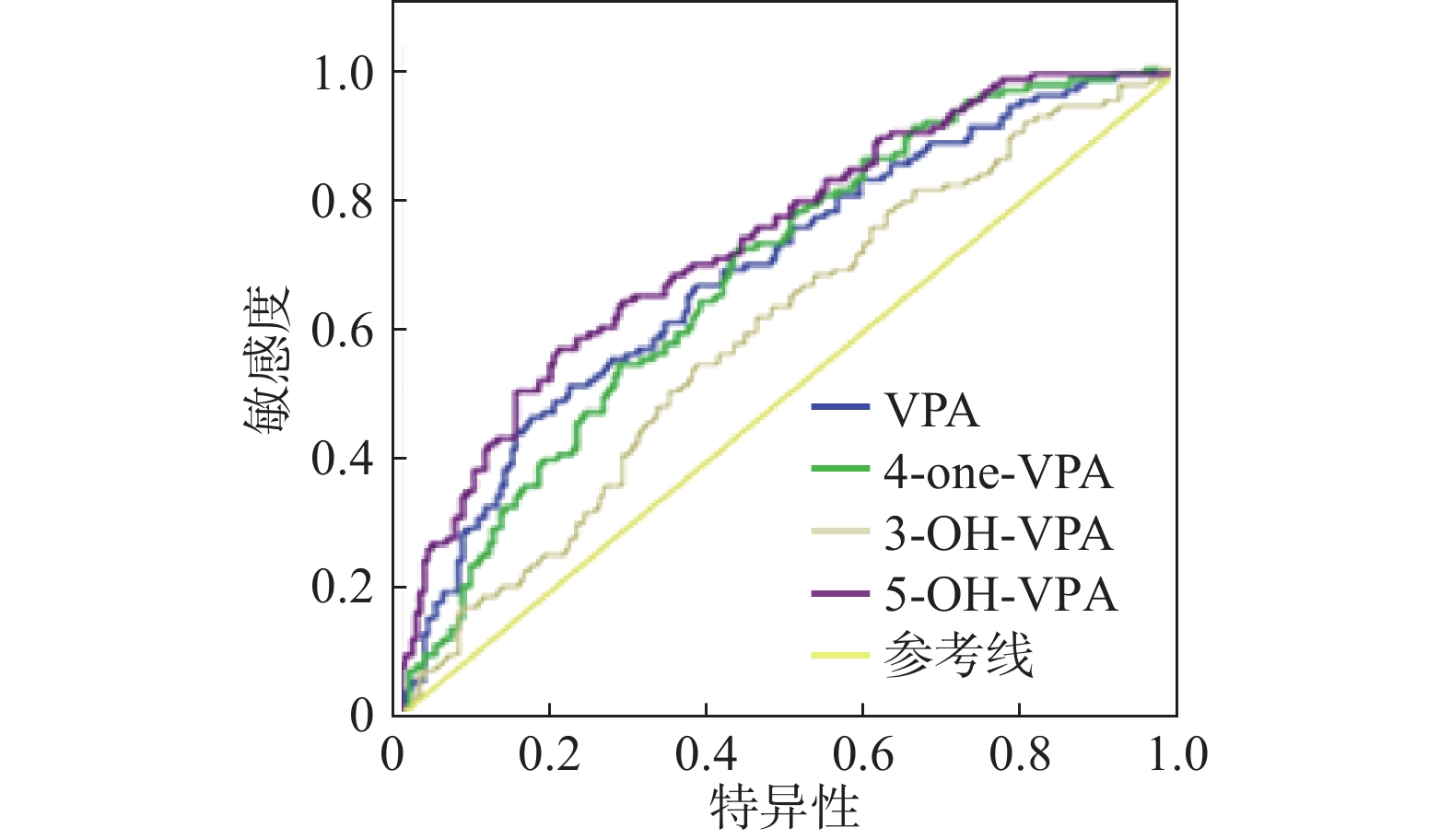
从本研究收集的123例肝功能异常者不同血药浓度分布(表2)可以看出,未超过中毒血药浓度而产生肝毒性的患者占69.10%,超过中毒血药浓度而产生肝毒性的患者占30.90%。结果表明:仅检测VPA血药浓度可能不能及时发现肝毒性不良反应的发生,因此考虑代谢产物的血药浓度是否可作为诊断肝损伤的参考指标。以VPA及其3个代谢产物血药浓度为变量做受试者工作特征曲线(receiver operating characteristic curve,ROC),检测其诊断肝毒性损伤的能力,因ROC曲线不受患者患病率的影响,对临床诊断具有研究意义。对VPA及其3个代谢产物进行ROC曲线作图,可看出ROC曲线下面积分别为0.690、0.682、0.594和0.736,均大于0.5,P值均小于0.05,说明VPA及其3个代谢产物可以用于肝毒性的诊断。因此,通过同时监测VPA及3个代谢产物的血药浓度能更好地预警肝毒性不良反应的发生,及时调整癫痫患者VPA的剂量,为临床合理化用药提供帮助。结果见表2、表3、图1。
血药浓度(μg/ml) 肝功能异常例数(%) <50 21(17.07) 50~100 64(52.03) >100 38(30.90) 组别 AUC 标准偏差 P值 95%置信区间 下限 上限 VPA 0.690 0.030 <0.001 0.631 0.748 4-ene-VPA 0.682 0.039 <0.001 0.625 0.74 3-OH-VPA 0.594 0.032 0.004 0.532 0.657 5-OH-VPA 0.736 0.028 <0.001 0.681 0.791
3.1. 肝功能正常与异常的癫痫患者血药浓度比较
3.2. 丙戊酸钠及其代谢产物对肝毒性相关性分析
-
VPA在体内药动学复杂,治疗窗窄,个体差异大,其毒副作用与其血药浓度相关,本研究对肝功能正常与异常的癫痫患者的VPA及其3个代谢产物血药浓度与肝毒性进行相关性分析,结果显示:肝功能异常组中VPA及其3个代谢产物的血药浓度均高于肝功能正常组患者,差异有统计学意义(P<0.05),提示VPA代谢产物中不仅4-ene-VPA血药浓度与肝毒性有关,3-OH-VPA和5-OH-VPA与肝毒性也有关系,同时监测VPA及其3个代谢产物血药浓度可以更好地预警肝毒性不良反应的发生。
本研究通过VPA及其3个代谢产物血药浓度为变量做ROC曲线,检测其诊断肝毒性损伤的能力,通过ROC曲线分析,VPA及其3个代谢产物的血药浓度均可作为诊断肝损伤的参考指标。其中,5-OH-VPA的ROC曲线下面积大于VPA。
综上,VPA及其3个代谢产物血药浓度均与肝毒性有关,这与课题组之前研究的VPA及其3个代谢产物对人体正常肝细胞体外肝毒性实验得到的结果一致,3-OH-VPA组和5-OH-VPA组差异更为明显。本研究还以VPA及其3个代谢产物血药浓度为变量做ROC曲线,检测其诊断肝毒性损伤的能力,5-OH-VPA大于VPA的ROC曲线下面积,结果提示临床可结合VPA及其代谢产物的血药浓度设计临床个体化给药方案,还可作为预警肝毒性不良反应发生的指标,为临床安全、有效给药提供参考。对于将VPA3个代谢产物作为标志物用于临床肝毒性诊断,还有待加大样本量验证,以确保诊断的特异性。









 DownLoad:
DownLoad: