-
围术期疼痛管理是加速康复外科的核心内容之一[1],舒芬太尼是围术期疼痛管理最常用的μ-阿片受体激动剂,由于对内脏痛控制效果不佳及剂量相关性不良反应,影响了其在腹腔镜胃肠外科术后镇痛中的疗效[2-3]。羟考酮是新一代μ、κ-阿片受体激动剂,其κ-受体激动效应可以有效减轻内脏痛[3-4]。与舒芬太尼相比,羟考酮在腹腔镜胃肠外科围术期疼痛管理是否更具优势,目前前瞻性系统临床研究不多。本研究拟比较舒芬太尼与羟考酮在腹腔镜胃肠癌择期手术患者围术期的有效性和安全性,为临床疼痛管理实践提供参考。
HTML
-
本研究已通过海军军医大学附属长征医院伦理委员会批准,批件编号:CZEC(2015)-32,并在中国临床试验注册中心注册(注册号:ChiCTR- PR-16007775)。选择2016年4月至10月期间,在本院行腹腔镜胃癌或肠癌择期手术患者59例,年龄18~65岁,ASAⅠ-Ⅲ级,BMI 18~25,所有患者均为同一组手术医生;排除标准:阿片类药物过敏或长期服用阿片类药物病史;近2周内有呼吸系统感染或有其他严重心、肝、脑、肾等系统病史;术前确定有神经或精神系统疾病;患有晕动症等系统疾病以及不愿提供知情同意书者。采用可重现的随机数字生成法,将患者分为羟考酮组(O组)30例,舒芬太尼组(S组)29例。所有患者术前均签署麻醉知情同意书和试验知情同意书。
-
所有患者均未用术前药物。入室后建立液体通路,行桡动脉穿刺置管监测有创动脉血压、监测心电图、脉搏氧饱和度及脑电双频指数。麻醉诱导:静脉推注地塞米松5 mg,咪唑安定0.05 mg/kg,丙泊酚1~2 mg/kg,O组患者静脉推注羟考酮0.3 mg/kg,S组患者静脉推注舒芬太尼0.3 μg/kg,1 min后静脉推注苯磺酸顺阿曲库铵0.2 mg/kg,2 min后待肌松起效且脑电双频指数(BIS)低于60,行气管插管机械控制通气。术中采用静吸复合麻醉,靶控输注(TCI)丙泊酚血浆浓度1.5~2.5 μg/ml,七氟烷吸入浓度1%~1.5%,维持脑电双频指数(BIS)40~60。血压或心率超过基础值的20%,O组患者静脉推注羟考酮0.1 mg/kg,S组患者静脉推注舒芬太尼0.1 μg/kg。手术结束前30 min,O组患者静脉推注羟考酮0.1 mg/kg,S组患者静脉推注舒芬太尼0.1 μg/kg。手术结束前15 min,两组患者均静脉推注多拉司琼12.5 mg预防恶心呕吐。术后麻醉苏醒室(PACU)行疼痛评估,VAS>4分则行镇痛补救:O组患者静脉推注羟考酮0.1 mg/kg,S组患者静脉推注舒芬太尼0.1 μg/kg,两组均采用滴定给药。
-
在麻醉诱导前(T0)、气管插管前(T1)、气管插管即刻(T2)、气管插管后0.5 min(T3)、气管插管后5 min(T4)、手术切皮后5 min(T5)、术后气管导管拔除即刻(T6)、气管导管拔除后5 min(T7)、术后30 min(T8)、术后6 h(T9)、术后12 h(T10)、术后24 h(T11)、术后48 h(T12),共13个时间点采集数据,并评估主要指标和次要指标。
主要指标包括:①视觉模拟评分(VAS):在T7-T12时间点记录患者的VAS评分,0分为无疼痛,10分为极度疼痛、无法耐受;②术后PACU需要镇痛补救的次数。
次要指标包括:①焦虑视觉模拟评分:术前让患者在长为100 mm的直线上,根据其自觉焦虑程度在直线上作标记,0分为完全无焦虑,100分为极度焦虑[3];②心血管反应:记录T0-T8时间点患者的血压和心率;③Ramsay评分:记录T7-T12时间点患者的Ramsay评分,1分为烦躁,2分为安静合作,3分为嗜睡、听从指令,4分为睡眠状态能被唤醒,5分为呼唤反应迟钝,6分为呼唤不醒[3];④记录围术期不良反应的发生情况:包括麻醉诱导期呛咳、术后呼吸抑制(呼吸频率< 10次/min)、术后恶心呕吐及术后躁动(采用躁动评分RS:0分为基本无躁动;1分为轻度躁动,可听从指令;2分为中度躁动,需医护人员控制;3分为重度躁动,有危险性举动;RS≥2分为躁动发生)[3]。⑤麻醉苏醒时间:包括清醒时间、自主呼吸恢复时间以及拔管时间[3]。
-
应用SPSS20.0统计软件进行数据分析,计量资料以(
$\bar x \pm s$ )表示。两组计量资料如服从正态分布及方差齐性,采用两独立样本t检验;否则采用Wilcoxon秩和检验。涉及到不同组间及不同时间点比较采用重复测量资料的方差分析。计数资料以率或构成比表示,采用X2检验或Fisher确切概率法。以P<0.05表示差异有统计学意义。
1.1. 一般资料
1.2. 麻醉方法
1.3. 观察指标
1.4. 统计分析
-
两组患者组间比较,无统计学差异(P>0.05),见表1。
项目 O组(n=30) S组(n=29) 统计量 P值 性别(男/女) 22/8 19/10 0.425① 0.515 手术类型(胃/肠) 20/10 18/11 0.136① 0.712 吸烟(是/否) 14/16 12/17 0.167① 0.683 ASA分级(Ⅰ/Ⅱ/Ⅲ) 7/20/3 5/20/4 −0.672② 0.502 年龄(岁) 57.13±7.10 55.93±7.21 0.645③ 0.521 身高(l/cm) 167.97±8.03 165.34±6.64 1.364③ 0.178 体重(m/kg) 61.33±9.68 59.52±8.46 0.766③ 0.447 BMI(kg/m2) 21.67±2.53 21.71±2.33 −0.071③ 0.943 手术时间(t/min) 154.53±27.30 160.00±24.46 −0.809③ 0.422 焦虑视觉模拟评分 42.67±10.68 41.79±8.83 0.342③ 0.734 注:①X2检验:X2值;②非参数检验:Z值;③t检验:t值。 -
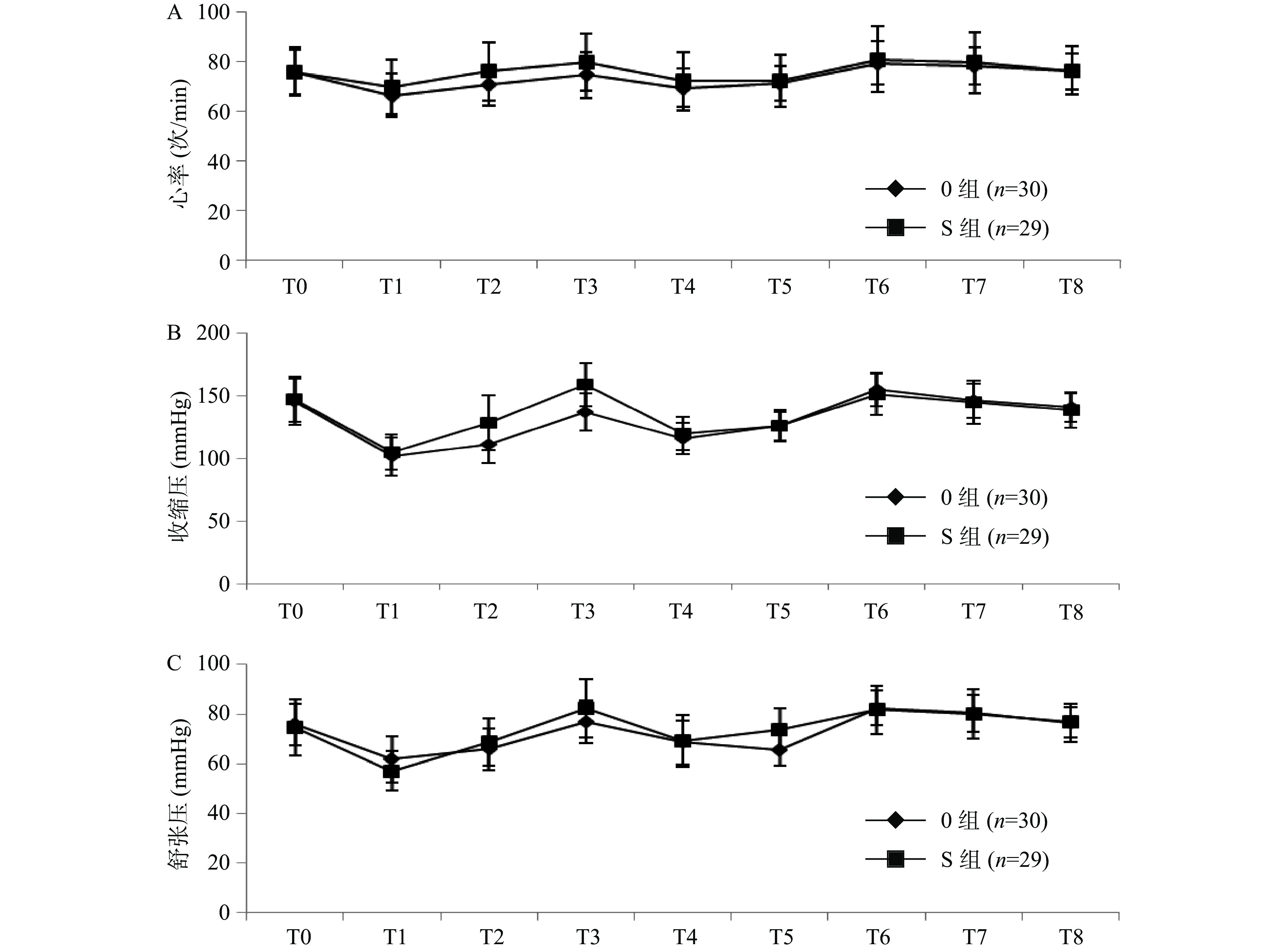
两组患者T0-T8收缩压(SBP)、舒张压(DBP)及心率(HR)组间比较无统计学差异(P>0.05),见图1。
-
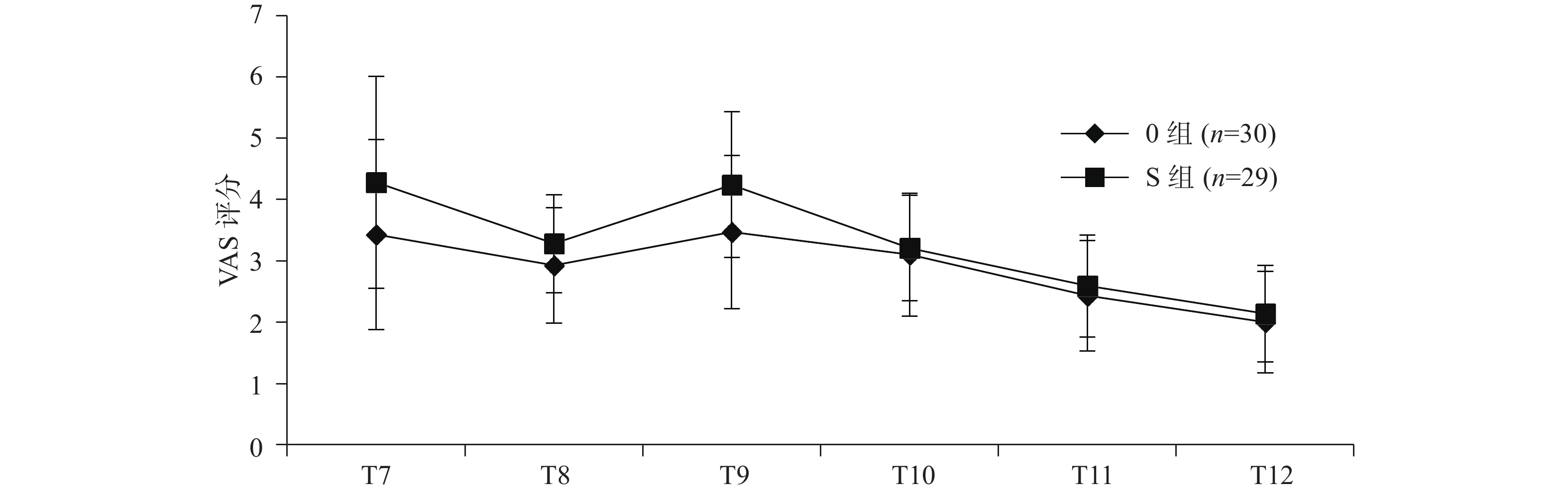
两组患者术后T7-T12 VAS评分组间比较无统计学差异(P>0.05),见图2。
-
两组患者术后PACU镇痛补救次数组间比较无统计学差异(P>0.05),见表2。
镇痛补救次数 O组(n=30) S组(n=29) Z值 P值 0 23 18 0.245 1 6 10 −1.161 — 2 1 1 — 注:“—”表示未取得。 -
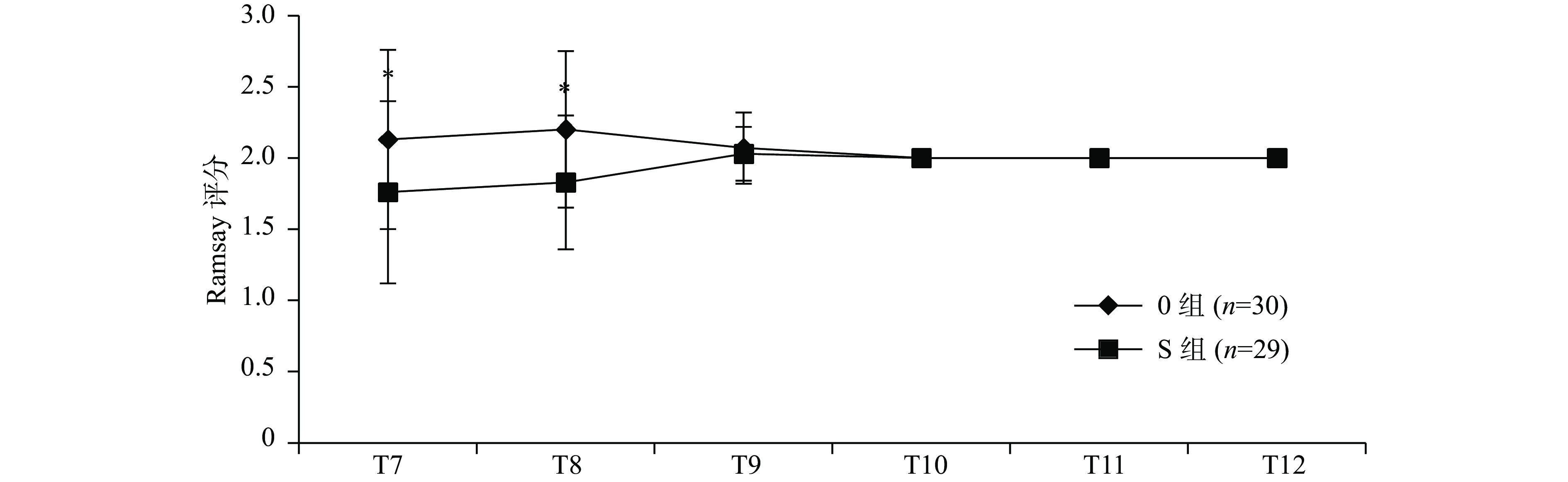
两组患者Ramsay评分组间比较,T7、T8差异有统计学意义(P<0.05),其他时间点差异无统计学意义(P>0.05),见图3。
-
两组患者组间比较,诱导期呛咳发生率O组显著低于S组(P<0.05);术后躁动发生率O组显著低于S组(P<0.05)。术后恶心、呕吐及呼吸抑制发生率无统计学差异(P>0.05),见表3。
不良反应 O组(n=30) S组(n=29) Χ2值 P值 恶心 8 6 0.291 0.590 呕吐 6 6 0.004 0.948 躁动 3 9 4.027 0.045 呼吸抑制 1 1 — 1.000 诱导期呛咳 0 6 9.228 0.002 注:“—”表示未取得。 -
两组患者睁眼时间、自主呼吸恢复时间和拔管时间组间比较无统计学差异(P>0.05),见表4。
观察项目 O组(n=30,t/min) S组(n=29,t/min) t值 P值 睁眼时间 17.13±3.15 18.55±4.14 −1.485 0.143 自主呼吸恢复时间 17.57±3.31 19.14±4.33 −1.569 0.122 拔管时间 20.53±3.48 21.66±4.58 −1.062 0.293
2.1. 一般资料
2.2. 心血管反应
2.3. VAS评分
2.4. 镇痛补救
2.5. Ramsay评分
2.6. 不良反应
2.7. 麻醉苏醒时间
-
本研究将舒芬太尼与羟考酮在腹腔镜胃癌或肠癌手术围术期应用的镇痛效应及不良反应进行比较分析发现:在麻醉诱导期,舒芬太尼组(S组)呛咳的发生率明显高于羟考酮组(O组)(P=0.02);麻醉诱导期呛咳可能导致胸内压、腹内压和眼内压增高,严重时可能导致患者心排血量下降和暂时性大脑局部供血不足,胸壁顺应性降低和声带闭合可能引起麻醉后通气困难[3, 5]。结合现有研究,考虑本研究中羟考酮组呛咳发生率低的机制可能为:①羟考酮能作用于延髓的咳嗽中枢而具有镇咳的效果[6];②舒芬太尼制剂中的枸橼酸成分可能刺激呼吸道肺C-纤维并最终作用于J-受体引发咳嗽,且呛咳的强度与枸橼酸的剂量相关[3, 7],而羟考酮制剂中不含枸橼酸成分,因此,麻醉诱导期应用羟考酮取代舒芬太尼,可以显著降低呛咳的发生率。
在麻醉苏醒期,本研究发现羟考酮组(O组)术后躁动的发生率显著低于舒芬太尼组(S组)(P=0.045);术后躁动是麻醉苏醒期最常见的并发症,表现为兴奋、烦躁和定向障碍,患者可出现烦躁、语无伦次等症状,严重时可能导致意外伤害甚至危及生命[8]。本研究中羟考酮组术后躁动发生率低的原因可能为:①有研究显示,腹腔镜胃肠癌手术患者术后躁动的发生可能与定位不明确的内脏痛相关[9],而羟考酮的κ-阿片受体激动效应可以有效减轻内脏痛,从而降低术后躁动的发生率;②羟考酮能够明显减少术后导尿管相关膀胱刺激症的发生率和严重程度,从而减少术后躁动的发生[3, 10];③本研究中羟考酮组在麻醉苏醒初期(T7、T8时间点)的Ramsay评分较舒芬太尼组高,其良好的镇静作用也是减少术后躁动的重要原因。同时,本研究比较羟考酮组和舒太尼组的睁眼时间、自主呼吸恢复时间和拔管时间,两组间差异无统计学意义,说明围术期应用羟考酮可以提供较好的镇静作用,且不影响麻醉苏醒时间。
在术后镇痛方面,羟考酮组(O组)与舒芬太尼组(S组)在术后T7-T12时间点的VAS评分、镇痛补救率两组间比较无统计学差异(P>0.05)。有研究显示:腹腔镜腹部手术的疼痛主要分为躯体痛和内脏痛[11],内脏痛范围弥散、定位不明确,患者往往主诉难受而非疼痛,且内脏痛在腔镜手术疼痛的发生中起主要作用[3,12],对内脏痛的控制不佳可能增加躁动等不良反应的发生率,但并不一定增加患者的疼痛评分;而躯体痛主要表现为浅表痛、伤口痛、可触摸的腹壁疼痛;舒芬太尼和羟考酮均是强效μ-阿片受体激动剂,对躯体痛均有较好的镇痛效果,所以两种药物在VAS评分和镇痛补救率方面比较无明显差别[3]。但在两组术中用药总量的比较中发现:羟考酮组术中用药总量为(0.41±0.03)mg/kg,而舒芬太尼组术中用药总量为(0.85±0.08)μg/kg。按照阿片类药物转化剂量表:吗啡:羟考酮:舒芬太尼=1:1:0.001来计算,羟考酮术中所需的药物用量较少,同时较少的阿片类药物用量也更有利于胃肠外科患者术后快速康复。但由于大量研究显示,硫酸吗啡生物利用度的个体差异较大,可达15%~64%,而羟考酮的生物利用度大于50%,因而在实际临床应用中,吗啡与羟考酮的等效剂量比可由1:1至1:2不等,所以阿片类药物临床实际转换与等效剂量表之间可能存在较大差别[13],因此,本研究未将两组患者术中阿片类药物用药总量换算为吗啡等效剂量来进行统计学的分析比较。
综上,我们的研究发现:羟考酮与舒芬太尼相比,前者可以明显减少腹腔镜胃肠外科手术患者诱导期呛咳和术后躁动的发生率,并提供良好的镇静作用。降低围术期麻醉相关不良反应的发生率以及良好的术后镇静,均有利于减少患者术后心理和生理的应激反应,对于胃肠外科手术患者快速康复具有重要意义。但是本研究亦存在一定的局限性:①未进行手术分层,后续研究应进一步区分讨论不同类型的腹部手术与药物疗效的关系;②本研究时间周期较短,样本量较小,因此可能难以发现某些研究结果的统计学差异,后续有条件可考虑开展多中心、大样本、前瞻性的随机对照临床试验[3]。








 DownLoad:
DownLoad: