-
细菌性脑膜炎是儿童时期常见的中枢神经系统急性感染性疾病,其病情重、进展快,病死率较高,即使治愈后常伴有不同程度的神经系统后遗症[1]。其最常见的病原菌是脑膜炎球菌、金黄色葡萄球菌和肺炎链球菌等。有效的抗菌药物治疗是细菌性脑膜炎治疗成功的关键,结合最新指南建议,规范临床用药,为患儿提供个体化治疗是临床药师关注的重点。本文通过对1例细菌性脑膜炎的个体化抗感染,对其药物治疗进行分析,为此类疾病的诊断和治疗提供参考。
HTML
-
患儿,女,13岁11个月,40 kg,主诉:因挤压鼻根部“青春痘”出现颜面部疼痛2 d,加重伴意识障碍1 d。入院前1 d疼痛加剧,双眼肿胀,伴低热,就诊于当地医院,予甘露醇、美罗培南联合万古霉素静脉滴注抗感染。治疗后,患儿仍烦躁不安,意识障碍进行性加重,遂以“颅内感染”收住我院。入院当天出现呼吸加快,伴高热,热峰39.6 ℃,逐渐出现意识不清。外院血常规:白细胞(WBC)25.4×109/L,中性粒细胞比例90.7%;血培养:革兰阳性球菌。入院查体:T 38.2 ℃,浅昏迷状态。面额部红肿,双眼睑张力高,双侧瞳孔不等,对光反射欠灵敏。颈强直,呼吸26次/min,双肺呼吸音粗,心率126次/min,心音有力,律齐。入院诊断:急性细菌性脑膜炎?
-
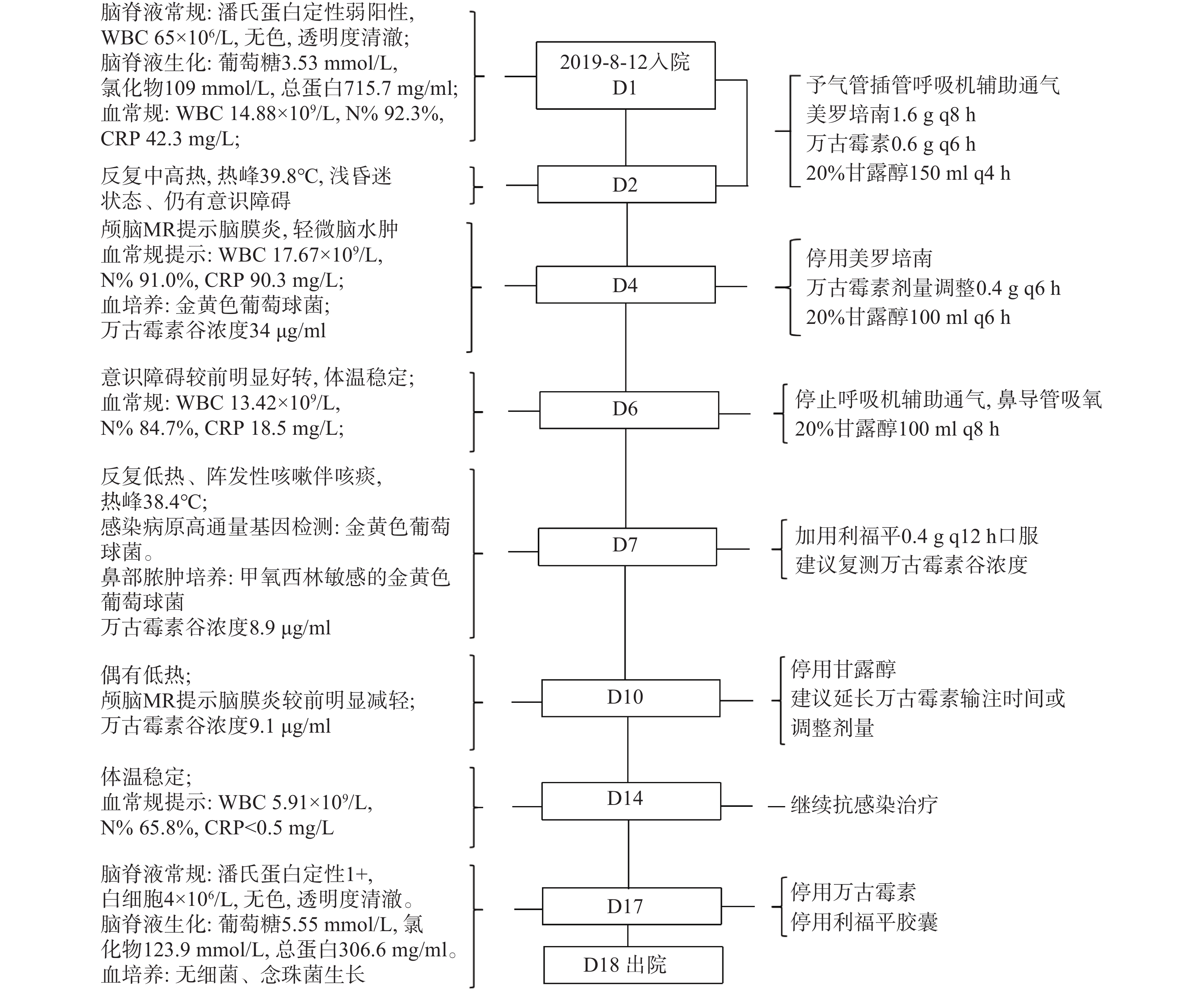
患儿于8月12日入院,有发热伴意识障碍,Glassgow评分6分,结合临床症状、体征及实验室检查结果,考虑细菌性脑膜炎,予美罗培南联合万古霉素治疗。D 4结合血培养结果及万古霉素药物浓度,药师建议更换药物为苯唑西林或调整给药剂量。D7反复低热,根据脑脊液病原高通量基因检测和鼻部脓肿培养结果加用利福平;D10万古霉素仍低于10 μg/ml,建议延长输注时间或调整剂量。D14病情有所好转,继续治疗。D18患儿病情稳定予以出院。住院期间重要的临床信息和治疗经过见图1。
1.1. 基本情况
1.2. 治疗经过
-
该患儿外院予美罗培南联合万古霉素治疗,可覆盖大多数病原菌,故继续使用两药治疗。对此药师分析:细菌性脑膜炎抗菌药物治疗的一般原则:①有效的杀菌作用。青霉素、美罗培南、万古霉素等对其常见致病菌如肺炎链球菌、流感嗜血杆菌、脑膜炎球菌等病原菌均有活性[2]。②穿透血脑屏障,能在脑脊液中达到足够的浓度。美罗培南能很好地进入脑脊液中达到有效浓度;万古霉素用于治疗脑膜炎时,在脑脊液中浓度可达9.13 mg/L[3-4]。美国传染病协会细菌性脑膜炎临床指南(IDSA)和《桑福德微生物治疗指南》第48版[5-6]均推荐美罗培南联合万古霉素用于细菌性脑膜炎的治疗。该患儿以美罗培南联合万古霉素为初始治疗是符合上述治疗指南的。
-
患儿血培养及药敏结果为金黄色葡萄球菌感染,对青霉素G耐药;对万古霉素、苯唑西林及利福平敏感(MIC值均≤0.5)。遵照儿童细菌性脑膜炎抗生素治疗规范及IDSA临床指南,对于金黄色葡萄球菌感染的脑膜炎,以苯唑西林为标准治疗,备选万古霉素[6-7]。故药师建议停用美罗培南,并将万古霉素改为苯唑西林,医师接受该建议,但苯唑西林未纳入我院常规药物目录,而临时采购可行性欠佳,故继续使用万古霉素。D7患儿仍反复低热,此外,鼻部脓肿培养及药敏结果为对甲氧西林敏感的金黄色葡萄球菌,对利福平敏感(MIC值≤0.5)。脑脊液病原高通量基因检测提示:金黄色葡萄球菌。结合上述检查结果,建议加用利福平。
-
由于万古霉素的治疗剂量与中毒剂量相近,个体差异较大,需监测万古霉素的血药浓度,及时调整剂量,实现个体化给药,避免不良反应的发生。本例患儿万古霉素初始给药:15 mg/kg q6 h。根据万古霉素个体化临床药师指引和加拿大儿科学会(CPS)超过1月疑似和确诊细菌性脑膜炎儿童患者的管理指南,万古霉素目标谷浓度为10~15 μg/ml[8-9]。D4患儿万古霉素血药谷浓度为34 μg/ml,谷浓度偏高,经验性将其剂量减为10 mg/kg q6 h。复测其谷浓度为8.9 μg/ml,低于10 μg/ml。虽然此时患儿发热间隔明显延长,但考虑低浓度易诱导耐药菌产生,建议复测万古霉素浓度,复测结果为9.1 μg/ml,仍偏低,建议增加单次给药剂量或延长输注时间,以提高谷浓度[10-11],但该建议未被采纳。
2.1. 细菌性脑膜炎初始治疗方案
2.2. 抗感染药物治疗方案调整
2.3. 万古霉素TDM及剂量调整
-
细菌性脑膜炎是儿童常见中枢神经系统感染,1月龄以上儿童常见致病菌为肺炎链球菌、脑膜炎球菌,而流感嗜血杆菌非常少见,李斯特菌罕见于青少年[6]。各指南[2, 5-6]推荐经验性治疗:首选头孢曲松联合万古霉素,备选:美罗培南联合万古霉素。患儿入院后考虑细菌性脑膜炎,经验性选择美罗培南联合万古霉素,初始治疗选择合理。血培养及脑脊液病原高通量基因检测结果示:金黄色葡萄球菌(青霉素G耐药)。文献报道金黄色葡萄球菌脑膜炎发生率逐渐上升,尤其是耐甲氧西林葡萄球菌引起的脑膜炎[12]。金黄色葡萄球菌感染的脑膜炎治疗推荐:以苯唑西林为标准治疗,备选万古霉素;青霉素过敏者可选用万古霉素联合利福平[7,13]。D7患儿病情虽然有所好转,但仍反复低热,鼻部脓肿培养及药敏结果:甲氧西林敏感的金黄色葡萄球,对利福平敏感(MIC值≤0.5)。利福平血脑屏障穿透性好,对金黄色葡萄球菌有活性,是治疗金黄色葡萄球菌脑膜炎的一个重要选择[14]。结合患儿病原学结果及药物获得性,存在联合使用利福平的依据,D14患儿病情好转。该患儿药敏结果提示病原菌对青霉素酶稳定的青霉素类、头孢类及碳青酶烯类敏感,头孢曲松脑脊液/血药浓度比为10~20%[2],治疗规范及指南中肺炎链球菌、脑膜炎奈瑟菌引起的脑膜炎的标准治疗推荐头孢曲松,在无法及时获得苯唑西林的情况下,能否考虑头孢曲松可作参考。
万古霉素治疗窗窄,TDM能显著增加临床有效率和降低肾毒性发生率。中国专家共识和欧洲临床微生物学和传染病学会细菌性脑膜炎指南[13,15]中指出,儿童应以15 mg/kg q6 h静脉滴注以达有效浓度。本例患儿按Schwartz公式估算肾小球滤过率为120.94 ml/min·1.73 m2,初始给药剂量符合指南推荐。指南[5, 14]推荐万古霉素有效血药谷浓度应在15~20 μg/ml,而加拿大CPS指南[9]推荐10~15 μg/ml,略低于前者。该患儿首次万古霉素血药谷浓度为34 mg/L高于上限,降低给药剂量后两次复测谷浓度均低于10 μg/ml。一项关于万古霉素间断输注与持续输注比较的Meta分析提出:万古霉素持续输注更易达到目标浓度,并更安全[10]。万古霉素属于时间依赖性抗菌药物,持续静脉输注时,血浆药物浓度可达到良好的药代/药效动力学指标并减少肾毒性风险[16]。建议增加剂量或延长输注时间以保证血药浓度达到目标浓度。临床医师以患儿病情好转并稳定为由未采纳该建议。查询文献发现:部分新生儿/儿童患者稳态谷浓度未达到10 μg/ml时仍有效,而血药浓度增加会带来肾毒性风险,故推荐目标谷浓度为5~15 μg/ml,而对于严重MRSA感染成人患者则推荐10~20 μg/ml,同时万古霉素AUC0~24 h目标范围在400~650 mg·h/L[17]。因此谷浓度偏低于目标浓度但患儿临床表现好转时,不调整给药剂量或方式是否妥当有待商榷。临床治疗时应基于感染部位、感染程度、病原结果等情况综合评估特定患者适宜的谷浓度。
-
在本例细菌性脑膜炎患儿的治疗过程中,临床药师及时与临床医生沟通,结合指南并参考权威抗感染资料选择初始抗菌药物,根据药敏结果及患者临床表现及时调整抗感染方案。通过监测万古霉素血药浓度,给予使用的相关建议,对临床用药具有实际指导意义。







 DownLoad:
DownLoad: