-
鹦鹉热衣原体是在革兰染色阴性需氧细胞内寄生的病原体,主要宿主为鸟类,吸入鹦鹉热衣原体污染的气溶胶可致病,人际间传播较为罕见,主要通过接触鸟类的排泄物感染,肺是主要受累器官之一,严重者可致呼吸衰竭[1]。重症肺炎又是一种起病急、进展迅速、病死率高、治疗困难且预后较差的呼吸系统疾病,是严重威胁人类生命健康的感染性疾病之一[2]。临床药师发挥药学专业优势,协助医师优化治疗方案,实施药学监护,提高合理用药和临床疗效。本文就临床药师参与1例鹦鹉热衣原体感染致重症肺炎并发药物性肝损伤老年患者的药学实践报道如下。
-
患者男性,83岁,身高178 cm,体重65 kg。2018-12-07因走路不稳,自觉发冷就诊于某医院急诊(神经内科),查胸部CT示右肺中叶见片状高密度影,边界不清,可见充气支气管影,血检验示血象、C反应蛋白(CRP)均升高,头颅磁共振等检查未见脑梗及脑出血征象,诊断为右肺中叶肺炎,予头孢唑肟(剂量不详)抗感染治疗。2018-12-09患者出现咳嗽、咳少量黄痰,呼吸短促,体温38.8℃,予以莫西沙星0.4 g qd联合头孢唑肟2.0 g q12h抗感染治疗。2018-12-09晚发热39.2℃并发房颤(房颤考虑莫西沙星不良反应),予亚胺培南-西司他丁钠0.5 g q8h抗感染,甲泼尼龙琥珀酸钠80 mg qd抗炎,低分子肝素钠抗凝等治疗。患者仍反复高热,气急加重,痰液不易咳出。2018-12-11复查胸部CT示右肺大片状密度增高影,血气分析示Ⅰ型呼吸衰竭,血象、CRP较前明显升高,加用替考拉宁(剂量不详)抗感染。但仍反复发热,氧合持续恶化。2018-12-12为进一步治疗,以“重症肺炎”转入呼吸重症监护病房。
既往史:患者有糖尿病史,自诉饮食控制,血糖控制尚可,否认其他病史。
辅助检查:①2018-12-07胸部CT:右肺中叶见片状高密度影,边界不清,可见充气支气管影。心脏彩超:右心房、左心室体积增大,心包见少量积液。诊断为右肺中叶肺炎。2018-12-11胸部CT:双肺见斑片状大片状密度增高影,双侧胸腔少量积液。②2018-12-09心电图:心房颤动伴快速心室率,左前分支传导阻滞。③2018-12-12血气:吸氧10 L/min,pH 7.31,PCO2 49.9 mmHg,PO2 69 mmHg,Hct 46%,SO2 96.6%,SBE 1.3 mmol/L。
入院诊断:①重症肺炎,双侧 PSI 183分,Ⅰ型呼吸衰竭;②Ⅱ型糖尿病。
-
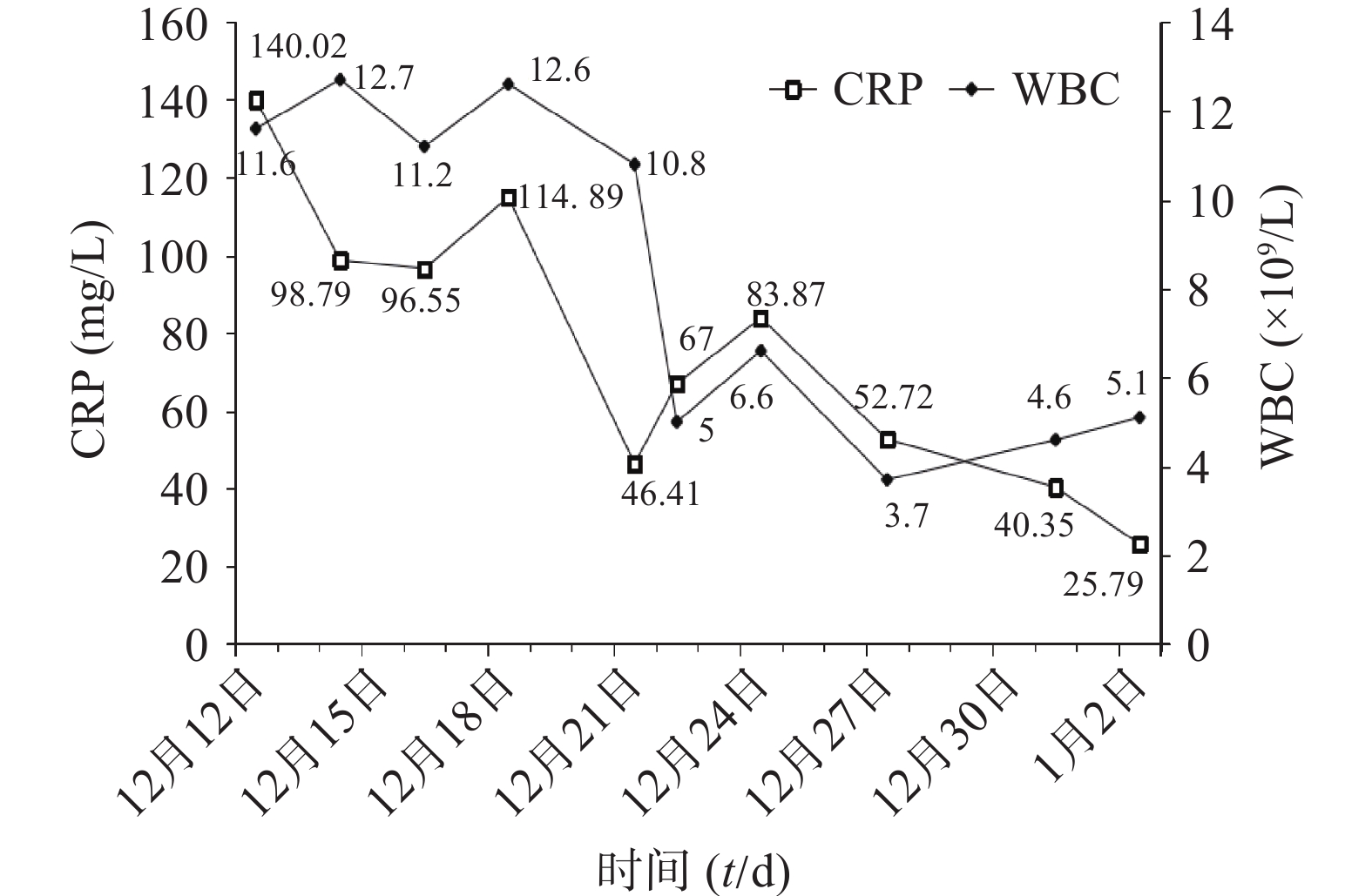
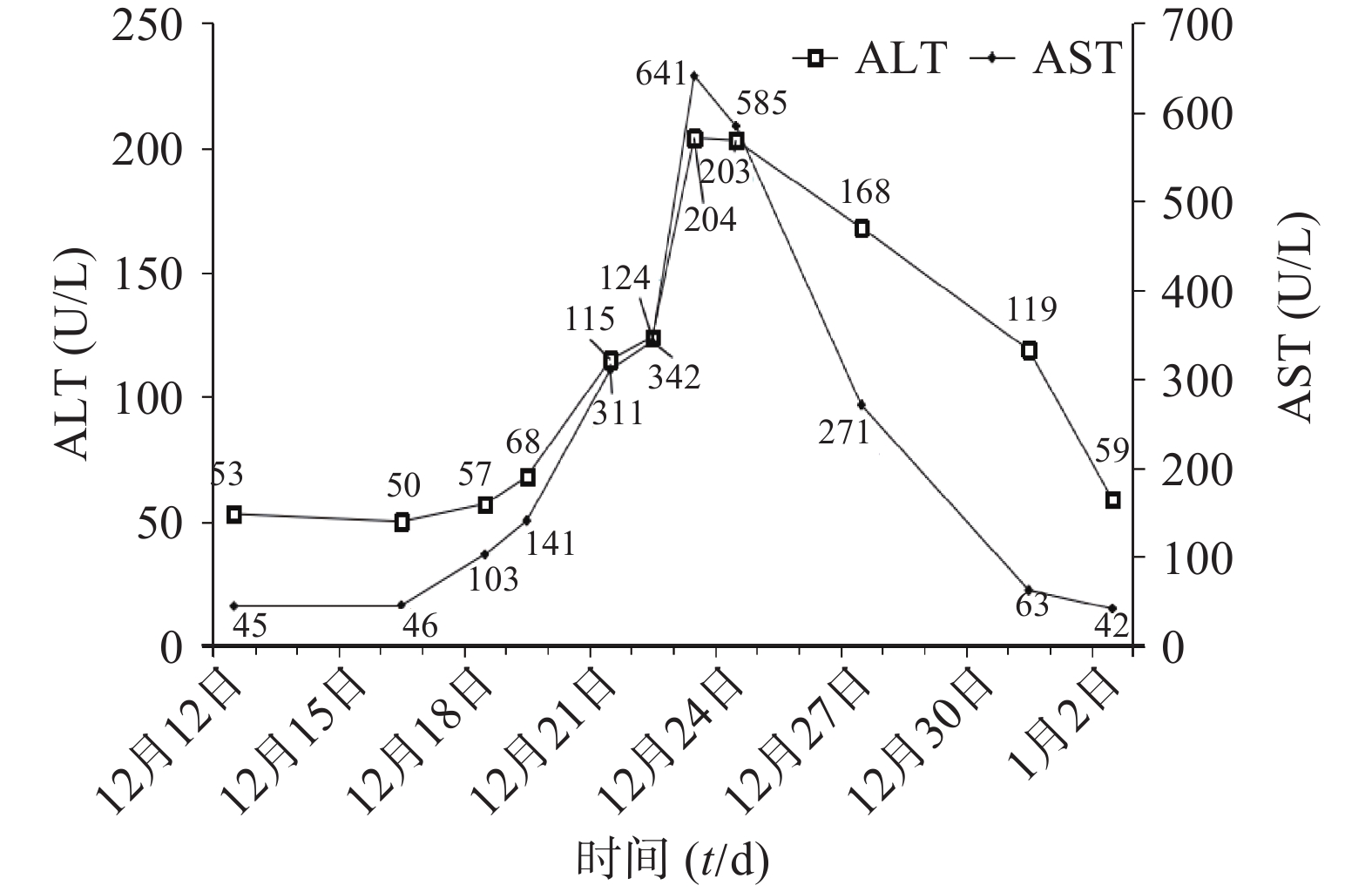
患者入科后完善相关检查(血常规、肝肾功能、电解质、血气、CRP)等,抗感染治疗前留取血培养、痰培养、尿培养行病原学检查。初始经验性予替考拉宁0.2 g qd ivgtt联合亚胺培南-西司他丁钠0.5 g q8h ivgtt抗菌治疗,同时予抗凝、营养支持、补液等对症支持治疗。12月14日(D3),体温较前升高,最高39.1℃,血常规:白细胞(WBC)12.7×109/L,中性粒细胞百分比(N%)95.9%,CRP 98.79 mg/L。呼吸机有创通气,气管镜检查:咽喉部较多黄色痰痂形成,黏膜充血,水肿较明显,尤以右侧气管主支气管及各级支气管炎性改变。患者感染加重,医师和药师共同讨论后,方案调整为亚胺培南-西司他丁钠0.5 g q6h ivgtt联合利奈唑胺0.6 g q12h ivgtt。12月16日(D5),Tmax 39℃,血常规:WBC 11.2×109/L,N% 96.9%,CRP 96.55 mg/L。双肺呼吸音粗,湿啰音较前加重,胸部X线:双肺炎症较前进展。气道分泌物基因二代测序结果回报:鹦鹉热衣原体序列数38。气道吸出物普通培养:白念珠菌。抗感染方案调整为阿奇霉素0.5 g qd ivgtt、多西环素0.1 g q12h 胃管注入(首剂加倍)、氟康唑氯化钠0.4 g qd ivgtt。12月21日(D10),Tmax 37.4℃,化验报告:WBC 10.8×109/L,N% 93.4%,CRP 46.41 mg/L,总胆红素(TBIL)18.4 U/L,丙氨酸氨基转移酶(ALT)115 U/L,天门冬氨酸氨基转移酶(AST)311 U/L。气管吸出物有少量白念珠菌,1,3-β-D葡聚糖检测结果正常,胸部X线:右肺炎症,较前有所吸收。评价治疗有效。但患者肝酶水平持续升高,分析可能药物性肝损伤(DILI),加用多烯磷脂酰胆碱232.5 mg qd ivgtt联合异甘草酸镁200 mg qd ivgtt保肝治疗。12月22日(D11),Tmax 37℃,化验报告:WBC 5×109/L,N% 70.9%,CRP 67 mg/L,ALT 124 U/L,AST 342 U/L,仍维持原方案治疗。12月23日(D12),Tmax 37.7℃,气道吸出物未培养出白念株菌,ALT 204 U/L,AST 641 U/L,ALP 82 U/L,INR 1.79。患者肝酶急剧升高,抗感染方案调整为多西环素0.1 g q12h联合克拉霉素0.5 g q12h,密切监测患者肝功能。1月2日(D22),感染基本控制。出院后继续予多西环素片治疗同时水飞蓟宾葡甲胺片保肝,1周后经回访,预后良好。
其住院期间WBC、CRP指标变化见图1,肝功能变化见图2,主要治疗药物见表1。
药物 D1 D2 D3 D4 D5 D6 D7 D8 D9 D10 D11 D12 D13 D14 D15 D16 D17 D18 D19 D20 D21 D22 亚胺培南-西司他丁钠 0.5 g q8h 0.5 g q6h 替考拉宁 0.2 g qd 利奈唑胺 0.6 g q12h 氟康唑氯化钠 400 mg qd 阿奇霉素 0.5 g qd 多西环素片 0.1 g q12h 克拉霉素片 0.5 g q12h 多烯磷脂酰胆碱 232.5 mg qd 异甘草酸镁 200 mg qd -
患者重症社区获得性肺炎,据《中国成人社区获得性肺炎诊断和治疗指南(2016年版)》[3](简称《指南》)和《中国急诊重症肺炎临床实践专家共识》[4]指出,重症肺炎致病菌未能明确时,推荐广谱抗菌药物治疗。初始经验予替考拉宁0.2 g qd ivgtt覆盖G+菌,包括甲氧西林耐药的金黄色葡萄球菌(MRSA),亚胺培南-西司他丁钠0.5 g q8h ivgtt覆盖G-菌,包括产酶耐药菌,从药效学的角度考虑,选药合理。根据《替考拉宁临床应用剂量专家共识》[5],替考拉宁的血清蛋白结合率高,用于肺部感染时,推荐起始负荷剂量为400 mg(或6~12 mg/kg)q12h ivgtt,连用3次,维持剂量为6~12 mg/kg qd ivgtt,该患者肾功能正常,无需调整剂量,根据体重换算,替考拉宁0.2 g qd ivgtt剂量不足,建议给予负荷剂量,维持剂量调整为0.4 g qd ivgtt,医师考虑急诊科已使用过该药,暂不予负荷剂量,且患者年龄较大,有糖尿病史,肾功能指标处于正常范围下限,从安全性考虑,维持剂量仍给予0.2 g qd ivgtt,暂未采纳建议。3 d后,感染加重,医师和药师分析可能原因:①替考拉宁使用剂量不足。②存在MRSA或多重耐药的G+菌感染。考虑到利奈唑胺分子量小,组织穿透力强,肺泡中浓度较高,药师查阅资料发现利奈唑胺治疗G+菌感染尤其是MRSA的有效率及细菌清除率优于替考拉宁,肾功能不全和皮疹的不良反应发生率低于替考拉宁[6-8],但应注意监测患者的血小板、呕吐或腹泻的不良反应[9]。综合治疗效果和安全性考虑,将替考拉宁更换为利奈唑胺。根据《抗菌药物药代动力学/药效学理论临床应用专家共识》[10],重症感染时,亚胺培南-西司他丁钠可增加给药次数或延长滴注时间,以提高药物浓度超过最低抑菌浓度(MIC)的时间占给药间隔的百分率(%T>MIC)。同时,为达到优化治疗的目的,亚胺培南-西司他丁钠用法调整为0.5 g q6h ivgtt。
入院第5天,二代基因测序和气道吸出物培养分别提示鹦鹉热衣原体和白念珠菌感染。《指南》[3]推荐鹦鹉热衣原体感染首选多西环素、米诺环素。文献[11-12]报道,阿奇霉素治疗鹦鹉热衣原体感染的重症肺炎临床效果较好,亦有报道[1]对于鹦鹉热衣原体四环素类是一线治疗。考虑阿奇霉素和多西环素分别作用于核糖体50S和30S亚基,合用可起到协同作用。经查阅文献未发现四环素类联合大环内酯类治疗鹦鹉热衣原体感染的重症肺炎,但有研究表明[13-14]多西环素联合阿奇霉素治疗支原体肺炎的临床效果明显优于单药治疗。阿奇霉素联合多西环素治疗支原体或衣原体感染的非淋菌性尿道炎疗效优于阿奇霉素单药治疗,降低血清中炎症因子的表达,且不会增加不良反应[15]。该患者呼吸衰竭,感染较重,故采用阿奇霉素联合多西环素抗鹦鹉热衣原体治疗,感染控制较好,药师认为此方案合理,可为今后鹦鹉热衣原体重症肺炎患者临床治疗提供参考。
患者气道吸出物培养为白念珠菌,念珠菌是常见的院内条件致病菌,该患者为重症监护患者,行气管插管,免疫力低下,有糖尿病等基础疾病,应予抗真菌治疗。《中国成人念珠菌病诊断与治疗专家共识》[16]推荐选择棘白菌素类药物、氟康唑、伏立康唑或两性霉素B及脂质体。综合患者情况及经济因素,予氟康唑氯化钠0.4 g qd ivgtt。5 d后疗效评价,患者症状及感染指标好转,抗真菌治疗有效,继续维持治疗。
入院第8天至第11天,患者肝酶进行性升高(图2)。药师分析,感染已好转,可排除疾病引起的肝酶升高[17],且无肝炎相关病史及酒精滥用史,可能为DILI。有研究[18]表明抗感染药物(6.08%)是继传统中药/膳食补充剂(26.81%)、抗结核药物(21.99%)、抗肿瘤药物或免疫调节剂(8.34%)之后第4位引起DILI的药物。根据《EASL临床实践指南:药物性肝损伤(2019年)》[19],采用RUCAM量表,判断多西环素、阿奇霉素和氟康唑与DILI的关系为极可能。据《药物性肝损伤诊治指南(2015年)》[20]指出,发生DILI时,应权衡患者病情及用药利弊决定是否停用可疑药物。入院第12天,ALT(204 U/L)>3×ULN(ULN:参考值上限),且INR(1.79)>1.5,达到停药标准。考虑多种药物合用会增加肝脏负担,且抗真菌治疗已1周,患者感染症状明显好转,停用氟康唑。由于抗鹦鹉热衣原体治疗周期较长,保留一线药物多西环素,研究表明[21],克拉霉素的肝胆系统的不良反应低于阿奇霉素,最终抗感染方案调整为多西环素联合克拉霉素。10 d后,患者肝功能、炎症指标基本恢复正常。
-
根据《药物性肝损伤诊治指南(2015年)》[20],基于受损靶细胞类型的分类,该患者ALT(204 U/L)>3×ULN,且R(5.31)>5[R=(ALT实测值/ULN)/(ALP实测值/ULN)],为肝细胞损伤型DILI,可选用抗炎、肝细胞膜修复、解毒类保肝药。异甘草酸镁是第4代甘草酸制剂,NMPA批准治疗ALT急剧升高的急性肝细胞型或混合型DILI,有效减轻炎性细胞浸润及肝细胞变性、坏死[22]。多烯磷脂酰胆碱是肝细胞膜的天然成分,通过影响膜结构使受损的肝功能和酶活力恢复正常,促进肝组织再生。该患者肝损伤进展较快,解毒类还原型谷胱甘肽起效较慢[23],建议多烯磷脂酰胆碱联合异甘草酸镁保肝治疗,医师采纳。
-
患者此次治疗过程中抗菌药物应用较多。利奈唑胺最常见的不良反应为骨髓抑制。替考拉宁具有耳、肾毒性,滴注过快会引起红人综合征。氟康唑和阿奇霉素合用,可导致QT间期延长风险增加。异甘草酸镁可引发假性醛固酮增多症,长期或大剂量使用,可引起低钾血症、水钠潴留及体重增加。药师密切监护,均未出现上述不良反应。多西环素、氟康唑、阿奇霉素、克拉霉素均有肝损伤的不良反应,监护期间发现患者肝酶进行性升高,药师结合患者病情,查阅资料,协助医师及时调整治疗方案,最终,感染控制,肝酶基本恢复正常。
患者服用多西环素片,应大量水送服,并保持体位直立30 min以上,用药期间不要直接暴露于阳光或紫外线下,一旦皮肤有红斑应立即停药。水飞蓟宾葡甲胺片偶可引起头晕、上腹部不适等反应,如不耐受,请及时就医。用药期间注意发生二重感染,定期随访血常规、肝功能及胸部CT。患者是养鸟爱好者,应注意保持养鸟环境卫生,在清洁粪便时,提倡应用“湿式作业”,以免微生物扩散到空气中,被吸入人体而感染。
Treatment and pharmaceutical care of one patient with Chlamydia psittaci pneumonia complicated by drug-induced liver injury
doi: 10.12206/j.issn.1006-0111.202103043
- Received Date: 2021-03-19
- Rev Recd Date: 2021-06-16
- Available Online: 2021-12-27
- Publish Date: 2021-11-25
-
Key words:
- Chlamydia psittaci /
- severe pneumonia /
- antimicrobial agents /
- drug-induced liver injury /
- pharmaceutical care
Abstract:
| Citation: | HU Yunying, FENG Jin, JIA Yao, GE Jiyun, BAO Leilei, HUANG Yufeng. Treatment and pharmaceutical care of one patient with Chlamydia psittaci pneumonia complicated by drug-induced liver injury[J]. Journal of Pharmaceutical Practice and Service, 2021, 39(6): 552-556. doi: 10.12206/j.issn.1006-0111.202103043 |







 DownLoad:
DownLoad: