-
化脓性血栓性静脉炎(STP)是指伴有细菌或真菌感染的血管内血栓形成[1],属于复杂性导管相关性血流感染并可引起局部或远处感染性并发症,在其治疗过程中抗菌药物的选择及使用具有关键作用[2]。此外,对于STP的抗凝治疗目前尚无统一认识,不同的医生选择也不尽相同[3]。STP虽不常见,但如果治疗不及时,会导致极高死亡率。本文从1例STP继发肺部感染患者的治疗过程,探讨合理抗感染及联合抗凝的必要性,并分析临床药师在重症医疗团队中开展药学监护的作用。
-
患者,男,17岁,身高165cm,体重65kg。2天前无明显诱因出现右下腹痛,伴恶心、呕吐,呕吐物为胃内容物,凌晨腹痛、呕吐加重,不能耐受,急诊至我院。实验室检查:白细胞(WBC) 6.41×109/L,中性粒细胞比率(N%) 84.1 %,C反应蛋白(CRP) 222.8 mg/L,降钙素原(PCT) 7.2 ng/ml,D-二聚体 9.17 mg/L,血肌酐(Scr) 114.1 μmol/L。影像学检查:腹部CT见少量腹水,大网膜及肠系膜增厚肿胀,盲肠及阑尾区域混杂密度占位,周围小淋巴结显示需排除阑尾炎伴周围脓肿。急诊以“急性化脓性阑尾炎”收治入院。患者先天性唐氏综合征,无其他特殊个人史及家族史。患者入院后病情进展迅速,出现呼吸、循环不稳定,肾脏损伤,经积极扩容补液后血压仍需大剂量去甲肾上腺素维持。急性生理与慢性健康评分(APACHE II)为14分,序贯器官衰竭检测评分(SOFA)为12分。
入院检查:腹膨隆,腹壁硬,全腹压痛,有肌紧张及反跳痛。体温38.2 ℃,心率160次/min,血压110/67 mmHg(去甲肾上腺素1.09 μg/kg·min),呼吸22次/min,血氧饱和度99%(呼吸机支持)。WBC 26.90×109/L,N% 94.60%,CRP 145.6 mg/L,PCT >100.00 ng/ml,肌酐171.0 μmol/L,尿素 8.84 mmol/L,白介素-6 2850.00 pg/ml。
入院诊断:①脓毒性休克;②急性化脓性阑尾炎伴弥漫性腹膜炎;③唐氏综合征。
-
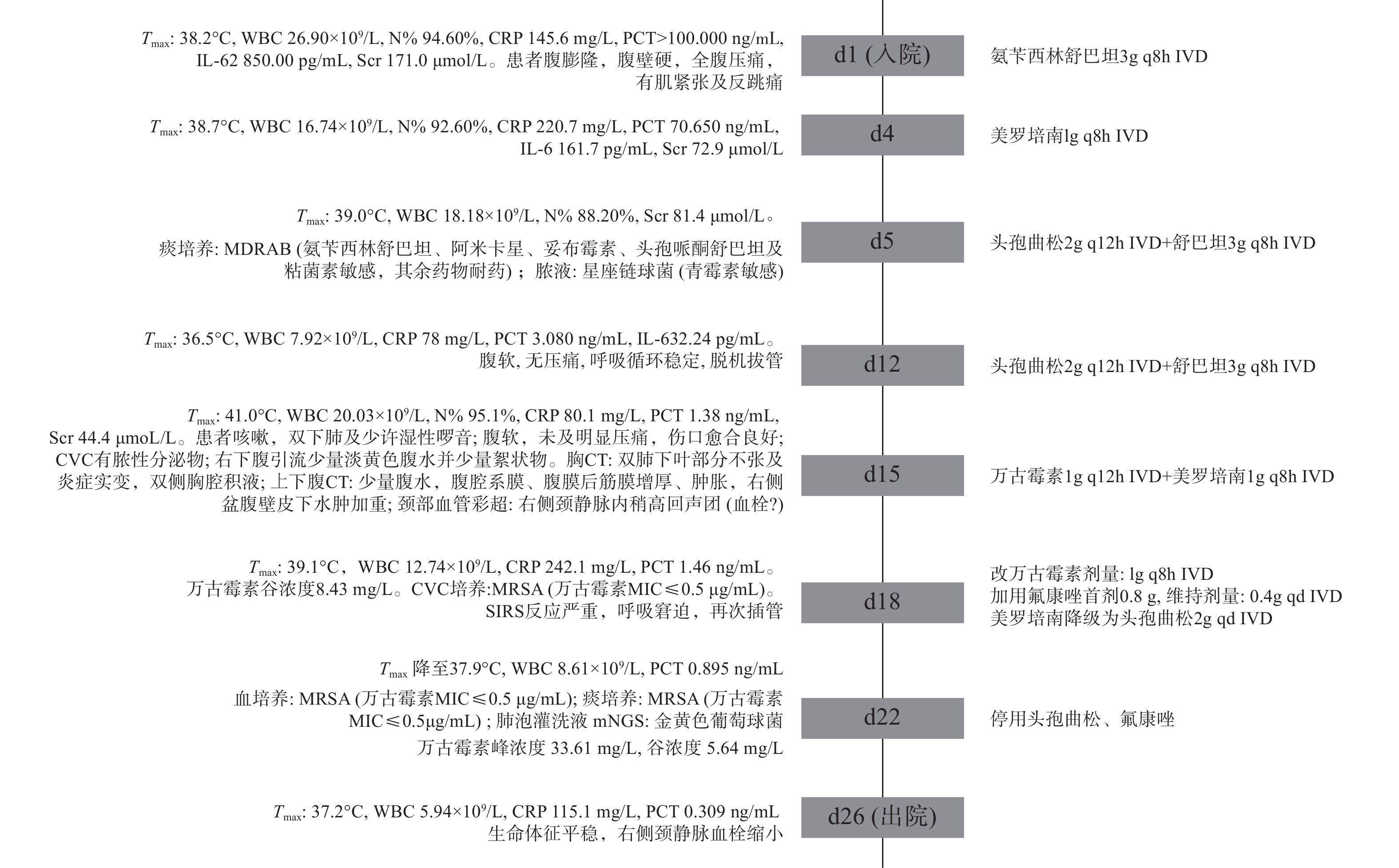
患者入院急行开腹探查术,术后转重症监护病房(ICU),呼吸机辅助通气、腹腔闭式引流改善腹腔顺应性、右侧颈内放置中心静脉导管(CVC),同时,液体复苏、血管活性药物维持血压并经验性抗感染治疗。入院第5 d,微生物学检查:多重耐药鲍曼不动杆菌(MDRAB)及星座链球菌感染。遂改用头孢曲松+舒巴坦,治疗6 d后,患者腹腔感染好转,血流动力学稳定,拔除气管插管。
入院第15 d,患者再次高热,留置导管处出现脓性分泌物且颈部血管彩超提示附壁血栓形成,胸CT提示双肺炎症。立即拔除CVC送血培养,当天CVC细菌涂片回报:少量革兰阳性球菌,升级抗感染方案,入院第18~21 d,分别从CVC、血培养、痰培养分离出耐甲氧西林金黄色葡萄球菌(MRSA),肺泡灌洗液宏基因组测序(mNGS):金黄色葡萄球菌。确诊MRSA导致复杂导管相关性血流感染,并继发肺部感染。根据患者症状体征、药敏试验结果及血药浓度监测结果等,调整抗感染治疗方案,同时辅以那曲肝素钙(0.4ml q12h ih)抗凝治疗。第26 d病情好转,患者及家属要求出院。住ICU期间重要临床信息及抗感染治疗经过见图1。
-
患者入院立即行腹腔引流及抗感染治疗,并于抗感染治疗之前,留送标本,但初始抗感染选用了氨苄西林舒巴坦。临床药师认为,社区获得性腹腔感染常见病原菌主要为肠道菌群,其标准抗菌治疗应包括抗肠杆菌、需氧链球菌、专性厌氧菌感染的药物[4]。目前全球革兰阴性肠杆菌科对氨苄西林舒巴坦的耐药性很强,从腹腔感染中最常分离出的10种细菌对氨苄西林舒巴坦均不敏感[5]。基于上述证据,且患者为重症感染,临床药师建议经验性抗感染药物更换为哌拉西拉他唑巴坦(4.5g q8h)或美罗培南(1g q8h),医师采纳。
-
患者入院第15 d,再次高热、脓毒症再袭,感染来源首先考虑导管,其次肺部,另外原发病灶也未完全控制,故调整抗感染方案为:万古霉素联合美罗培南。2 d后患者仍高热、气促、呼吸窘迫,临床药师分析抗感染疗效不佳的可能原因,并给出相应建议:①抗菌药物剂量不足,万古霉素个体化差异较大,建议监测万古霉素血药浓度以便及时调整[6]。②治疗方案未覆盖致病菌,根据念珠菌评分(CS),该患者目前4分(脓毒症2分、腹部手术1分、肠外营养1分),念珠菌感染风险较高,建议启动抗真菌抢先治疗。③患者微生物培养结果为革兰阳性菌且PCT< 2ng/ml, 耐药革兰阴性菌感染可能较小,美罗培南降阶梯为头孢曲松,避免长期使用广谱抗菌药导致二重感染。医师采纳临床药师建议。
入院第18~21 d,导管、血、痰培养均为MRSA,提示肺部感染继发于STP,以往研究也证明继发于STP的脓毒性栓子更常见于肺部[7],治疗应以血流感染为主同时兼顾肺部。在病原菌明确的情况下,药师建议停用氟康唑及头孢曲松。万古霉素在肺泡上皮衬液(ELF)中浓度/血药浓度为5%~50%,肺内分布良好,表明在治疗STP同时能在肺部达到有效治疗浓度,疗程需要延长至4~6周[8]
-
⑴万古霉素初始给药方案制订:患者初始给予万古霉素1g q12h,连续使用3 d疗效不佳。临床药师评估治疗方案后,发现未结合万古霉素的药动学/药效学(PK/PD)特点及重症患者的病、生理情况来设计给药,导致万古霉素未达到PK/PD目标靶值。根据《2020万古霉素治疗严重MRSA感染的治疗药物监测》共识指南[6],≥12岁儿科患者初始治疗剂量为60~70 mg/(kg·d),不超过3.6g 为宜,患者体重65 kg,初始给药剂量3~3.6 g/d较合适。指南同时推荐MRSA引起重症感染的成人患者给予负荷剂量以助于快速达到目标稳态浓度,控制感染,而儿科患者缺乏大型前瞻性研究,但回顾性研究提示接受万古霉素负荷剂量(20~25 mg/kg)的儿童与未接受的相比,可能更快达到初始目标谷浓度,且不增加肾毒性[9]。该患者近期高热、心率偏快,处于高代谢状态,且处于肾功能亢进状态(肌酐清除率220 ml/min),可能进一步加快万古霉素代谢,故临床药师认为该患者初始给药方案:首剂1.5g+维持1g q8h,更利于快速达标、控制感染,同时进行治疗药物监测,便于后续剂量调整。
⑵万古霉素剂量优化:第4 d万古霉素血药浓度监测结果为Cmin 8.43 mg/L,根据《中国万古霉素治疗药物监测指南》[10],对于严重MRSA感染的患者,建议万古霉素目标谷浓度维持在10~20 mg/L。因此,临床药师建议增加一个给药间隔,以提高药物血药浓度,并持续监测。治疗第6 d,万古霉素血药浓度:Cmax 33.61 mg/L,Cmin 5.64 mg/L,谷值依然未达标,但患者体温下降,症状及感染指标均好转,医生考虑抗感染治疗有效,询问临床药师是否需要调整万古霉素给药方案。临床药师经查阅最新共识指南[6],建议通过监测药物浓度-时间曲线下面积(AUC)来指导万古霉素的剂量调整,推荐个体化给药AUC/MIC目标值为400~600以达到最佳的临床疗效。同时文献[11]指出谷浓度可能不是AUC最佳替代,在几种不同剂量方案下AUC范围很宽,但可产生相似谷值;同样相似AUC,谷值也不尽相同。因此,临床药师根据所测峰谷浓度,依据线性梯形法则计算万古霉素AUC0-24为415 mg·h/L,故建议维持原剂量治疗。经密切监测患者肾功能并观察各项感染指标、体温情况,均持续好转,提示治疗有效且未发生肾功能损伤等不良反应。为此,临床药师建议万古霉素根据AUC调整更精确,相比单点暴露的谷浓度,AUC为累积药物暴露总量,以往是将谷浓度转化为每日最小AUC,存在一定局限性,尤其在重症患者中,药物代谢受多方面因素影响,谷浓度可能不足以指导所有患者的剂量调整,而AUC0-24h则代表该时间段的平均浓度,可更好体现目标实现率与疗效的关系,指导剂量优化。
-
导管相关性血流感染和血栓形成互为因果,导管周围出现血栓,亦增加了微生物定植和菌血症的风险[12]。关于化脓性血栓静脉炎是否给予全身抗凝治疗尚存在争议,由于STP很少见,缺少临床试验,无法研究可能的疗效和安全性结果或获益可能超过风险的亚群[13]。Uptodate[14]建议,STP采取抗凝治疗情况包括:在适宜抗生素治疗下血栓仍扩散;脓毒症在48~72 h的适宜抗菌药物治疗后仍不受控制;高凝状态。《2018美国血液病学会儿童静脉血栓栓塞症管理指南》指出抗凝或不抗凝都是合理的[15]。临床药师经查阅文献,提示颈静脉、门静脉血栓一般推荐在血栓扩大或经抗生素治疗后进展才抗凝治疗[13]。有学者[16]对28名STP住院儿科患者的抗凝治疗时间及安全性进行了为期10年的回顾性研究,其中25名患者接受抗凝治疗,疗程约12周,血栓清除率48%,尽管治疗结束时血栓溶解率较低,但感染复发风险低,没有发现延长抗凝的优势,同时抗凝安全性良好。
临床药师综合现有证据,建议仅在血栓扩展或复发的情况下考虑抗凝,疗程12周;抗凝的安全结局除出血,还应考虑到血栓破裂引起感染灶扩散及脓肿出血性转化。结合本例患者情况,STP诊断明确,肺部感染继发于STP,微生物培养得到证实,抗感染方案已优化,为进一步防止血栓扩散,可考虑抗凝。同时复查D-二聚体、血栓弹力图,评估患者出血与血栓风险,发现患者D-二聚体从入院开始持续升高至15.45mg/L,同时凝血因子活性升高,表明其血栓形成风险高,出血风险低。故临床药师建议抗感染同时给予那曲肝素钙0.4ml q12h。经过抗凝及抗感染治疗,患者右侧颈静脉附壁血栓缩小,未出现肺栓塞及感染性心内膜炎。
-
本病例患者初始因腹内脓毒症入院,经过积极引流、抗感染治疗后腹腔感染好转,但后期继发院内感染,导致脓毒症再袭。提示重症患者病情多变,临床药师需要时刻关注患者症状、体征的改变,并根据感染部位、严重程度及时调整抗感染方向。同时,重症感染患者治疗成功的关键在于确保抗菌药物给药剂量能达到PK/PD目标靶值,合理进行个体化血药浓度监测是调整并优化重症患者给药方案的基础,临床药师借助TDM,对于监测数据的准确解读及应用,实现了重症儿科患者的精准化治疗。化脓性血栓静脉炎治疗方案制订过程检索了国内外指南及文献,充分考虑了抗凝治疗的时机及必要性,保障了患者用药安全及疗效。
Analysis of drug therapy in a patient with pulmonary infection secondary to suppurative thrombophlebitis
doi: 10.12206/j.issn.1006-0111.202107045
- Received Date: 2021-07-16
- Rev Recd Date: 2021-10-18
- Available Online: 2022-03-29
- Publish Date: 2022-03-25
-
Key words:
- suppurative thrombophlebitis /
- metastatic infection /
- vancomycin /
- therapeutic drug monitoring /
- anticoagulation
Abstract:
| Citation: | QU Runan, MAO Junqin, XIN Rujuan, ZHANG He, GAO An. Analysis of drug therapy in a patient with pulmonary infection secondary to suppurative thrombophlebitis[J]. Journal of Pharmaceutical Practice and Service, 2022, 40(2): 171-174. doi: 10.12206/j.issn.1006-0111.202107045 |







 DownLoad:
DownLoad: