-
粒细胞集落刺激因子(G-CSF)是一种由单核细胞、巨噬细胞、成纤维细胞和内皮细胞产生的骨髓生长因子,可刺激中性粒细胞前体的增殖、终末成熟和存活,并动员骨髓中祖细胞到外周血中[1]。
重组人粒细胞集落刺激因子(rhG-CSF)为基因重组技术的产品,临床上广泛用于各种中性粒细胞减少症的治疗及预防,但在使用此类药物时必须考虑不良事件的风险。总体来说,虽然rhG-CSF在动物和人类研究中都被证明是相对安全的,常见的不良反应如疲劳、头痛和骨痛,但是,其存在诱导肺毒性的可能,有报告其用于中性粒细胞减少症恢复期间出现急性呼吸衰竭[2- 3]。但搜索国内外相关文献未发现其致嗜酸性粒细胞肺炎的报道,本文就1例因粒细胞缺乏患者经rhG-CSF治疗后出现急性嗜酸性粒细胞肺炎进行分析,并讨论其引起急性肺损伤的原因和治疗方案,为临床识别药物不良反应提供参考。
-
患者,男,73岁,身高170 cm,体质量50 kg。因乏力纳差2周,伴少量咳嗽,于我院就诊。急诊查胸部计算机断层扫描(CT)示肺气肿,双肺炎症;血常规示三系降低:白细胞2.2×109/L,血红蛋白46g/L,血小板11×109/L,8年前喉癌手术及放疗病史,目前腮腺功能受损。2021年4月2日入院初步诊断:重度贫血;肺部感染;喉癌术后。
入院体格检查:体温36.5 ℃,脉搏82次/min,呼吸21次/min,血压90/60mmHg。神志萎靡,全身皮肤黏膜苍白,严重贫血貌,浅表淋巴结未触及病理性肿大。呼吸运动正常,无胸膜摩擦感,双肺呼吸音清,未及干湿罗音。
-
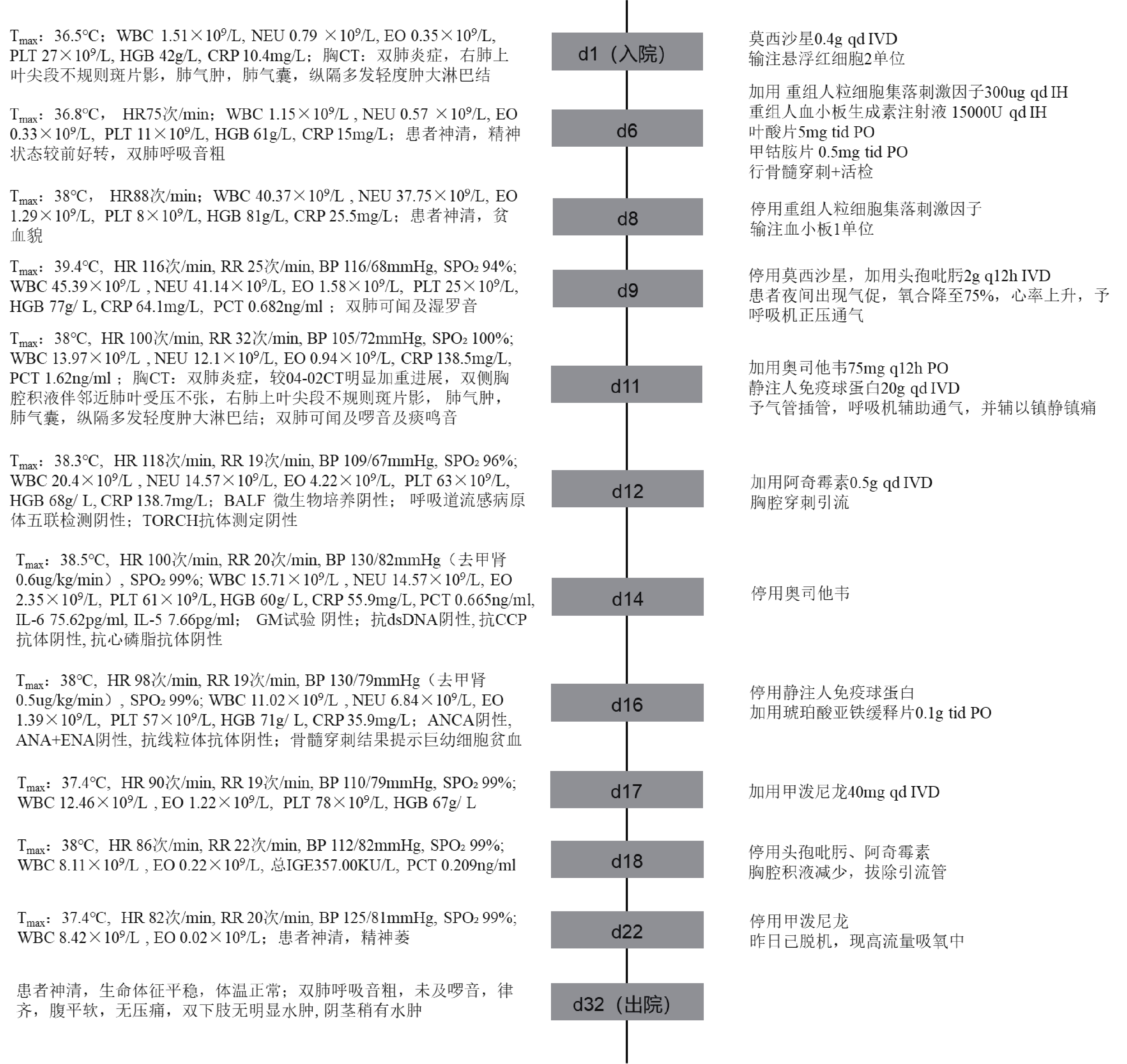
患者入院考虑社区获得性肺炎,给予莫西沙星抗感染;完善相关检查后诊断巨幼红细胞性贫血,输注悬浮红细胞,并予叶酸、甲钴胺片、琥珀酸亚铁缓释片治疗;同时输血小板、予重组人血小板生成素升高血小板;4月7日至4月9日,给予重组人粒细胞集落刺激因子300 µg升白细胞。
患者于4月8日出现发热,体温(T)37.5 ℃,4月10日升至39.4 ℃,呼吸频率加快(RR 22次/min),心率116次/min,考虑急性肺水肿,转入ICU。复查血常规示白细胞、嗜酸性粒细胞升高:WBC 45.39×109/L, EO 1.58×109/L。复查胸CT示间质性改变伴胸腔积液,纵隔多发轻度肿大的淋巴结,较4月2日症状明显加重。行无创通气后血氧饱和度持续降至75%,气促加重,予气管插管、呼吸机辅助通气,同时先后给予头孢吡肟、阿奇霉素抗感染治疗,奥司他韦抗病毒治疗,症状改善不明显。至4月18日患者仍持续发热,嗜酸性粒细胞仍较高,期间肺泡灌洗液(BALF)微生物培养阴性,呼吸道九联阴性,半乳甘露聚糖抗原(GM)检测阴性,抗核抗体(ANA)、抗双链脱氧核糖核酸(dsDNA)、抗环瓜氨酸肽抗体(CCP)、抗中性粒细胞胞浆抗体(ANCA)阴性、抗可提取性核抗原(ENA)均阴性,TORCH抗体测定阴性。结合患者病史、用药史,考虑为rhG-CSF相关的嗜酸性粒细胞肺炎,加用甲泼尼龙40 mg治疗5 d并停用抗菌药物。4月29日,复查CT提示患者双肺炎症较前好转,EO恢复正常,体温正常,于5月3日转康复医院继续治疗。住院期间重要临床信息及治疗经过见图1。
-
rhG-CSF罕见但严重ADR,包括过敏性休克、急性肺损伤、间质性肺炎、急性肾衰竭、严重精神异常等[4]。重组人粒细胞刺激因子注射液(协和发酵麒麟株式会社)说明书不良反应一项指出“有发生间质性肺炎或促其加重可能”。一项针对G-CSF诱导肺毒性的临床病例报告和实验数据的系统评价表明,其肺部常见ADR,包括咳嗽、呼吸困难、间质或肺泡浸润,伴有轻度至重度血气恶化[2]。日本关于药物性肺损伤诊断和治疗的共识声明指出,G-CSF制剂可诱发嗜酸性粒细胞性肺炎[5]。总之,rhG-CSF有引起药物性肺损伤的可能。
嗜酸性粒细胞性肺炎(EP)是药物性肺损伤的一种类型,以嗜酸性粒细胞增多和肺部浸润为特征的异质性疾病,根据病程可以分为急性EP(AEP)和慢性EP(CEP)。患者可出现急性呼吸道症状,如呼吸窘迫、低氧血症、咳嗽并对皮质类固醇的快速治疗反应[6]。外周血EO>1~1.5×109/L加上典型肺部影像学征象可协助做出诊断[7]。该患者使用rhG-CSF后,出现发热、呼吸困难、血氧饱和度下降等症状,给予抗细菌及抗病毒治疗无效。通过微生物学培养阴性、ANA+ dsDNA+ CCP阴性、ANCA及巨细胞病毒等阴性,结果排除了肺部感染、结缔组织病、血管炎。同时患者外周血EO升高,胸部CT示双侧肺浸润、纵隔淋巴结肿大、胸腔积液、小叶间隔增厚,总IgE及IL-5升高,支持EP的诊断。多种病因与EP相关,包括烟草烟雾、真菌感染、寄生虫感染、恶性肿瘤和药物[8]。该患者确实有吸烟史(每日1包),但AEP在新吸烟者中更常见,而CEP通常会影响非吸烟者[9];真菌和寄生虫病因分别被GM试验阴性和弓形体IgM阴性排除;患者有恶性肿瘤病史,但目前肿瘤标志物正常,影像学未提示肿瘤进展且EP在淋巴瘤患者更常见。患者接受的其他与EP相关的药物为阿奇霉素,但患者4月10号即出现急性症状,阿奇霉素4月13号才使用,缺乏时间相关性。
依据国家药物不良反应关联性评价标准,患者嗜酸性粒细胞增多与rhG-CSF使用呈正相关,与EP发生有合理的时间关系,肺损伤及EP是G-CSF已知罕见不良反应类型,EP不可用其他合并用药的作用及其他治疗的影响及患者病情进展来解释,故判断为“可能相关”。同时按照“诺氏不良反应评估量表”进行评估得6分,判断为“很可能相关”。
-
AEP 的发病机制尚不完全清楚,被认为与抗原免疫相关,可能由肺泡巨噬细胞呈递致病因子(过敏原、烟雾、药物)引发急性I 型超敏反应。G-CSF可能通过诱导辅助T细胞2型(Th2)免疫反应 [10-11],产生IL-5等细胞因子,诱导炎症级联反应,增加EO数量并促使其积聚到肺实质诱发急性I型超敏反应[12]。IL-5在AEP的发生过程中起着很重要的作用,骨髓和血液中EO的增多以及肺嗜酸性粒细胞浸润均依赖于 IL-5。本例患者也发现IL-5水平明显增加,IL-5不仅可维持骨髓中EO的产生,还能动员EO迁移到肺泡,延长其在组织中的寿命。另外在IL-5 存在的情况下,嗜酸性粒细胞趋化因子和 IL-13均可促进EO的产生及向肺部积聚[13-14],最终促进EO脱颗粒并释放储存介质,包括特定的颗粒蛋白,如主要碱性蛋白(MBP)、白三烯(cysLTs)、活性氧,它们在过敏性炎症部位积聚,促进该区域的炎症,损害气道内皮细胞和气管内膜,并可能对周围组织结构造成损伤[13]。
另外,有研究表明,中性粒细胞快速恢复是发生严重肺部不良事件的危险因素,在中性粒细胞减少症恢复期间,先前肺部受累可能会被加重[15]。因为骨髓发育不全后再生的成熟中性粒细胞具有功能活性,在适当激活时可产生氧自由基 [16],G-CSF则可能通过增加细胞因子的产生并激活循环或肺泡中性粒细胞和巨噬细胞内的氧化爆发(oxidative burst) 而加剧这种肺部不良事件的发生 [3, 17],因此,在原有肺部受累情况下使用G-CSF,可能存在呼吸状态恶化、急性肺损伤或呼吸窘迫综合征发生的风险。本例患者初始入院存在肺部感染,使用G-CSF快速升高中性粒细胞的同时很有可能导致功能性中性粒细胞与病原体、细胞碎片之间通过相互作用释放活性氧中间体和蛋白水解酶,刺激细胞代谢从而诱发肺损伤。
-
继发于药物引起的AEP,首先,立即停用任何可疑药物,如发生呼吸衰竭,应给予机械通气辅助呼吸并尽快开始糖皮质激素治疗。
糖皮质激素治疗的最佳剂量和时间尚无明确共识,常取决于疾病的严重程度。另外,EP通常对皮质类固醇有很好的反应,一般在开始治疗24~48 h症状可减轻,尤其在发病初期EO显著增多的患者中,短期糖皮质激素治疗亦可取得较好的疗效。一项研究表明[18]在初始EO增多的EP患者中使用皮质类固醇治疗中位时间为4 d,达到总体临床稳定的中位时间为3 d,与EO正常患者使用皮质类固醇治疗中位时间14 d相比,并未发生治疗失败,可能由于初始EO增加的患者病情更轻。Jhun[19]也观察到,发病初期外周血EO增多的患者,疾病程度普遍较轻,患者氧气需求量,供氧时间及ICU入住率也均较低。本例患者外周血EO在rhG-CSF刺激下迅速升高,但及时停用了rhG-CSF并使用甲泼尼龙治疗后5 d病情迅速改善。
-
药物引起肺损伤不常见,但需要警惕,尤其是突然出现或快速进展的肺部病变,不能用感染或其他常见病因解释时需要注意除外药物因素。由于药物引起的肺损伤其症状、体征、影像学表现无特异性,需结合药物使用、病史及辅助检查综合判断,停用引发肺损伤的药物并及时给予皮质类固醇治疗后肺部病变可以逆转,如果不及时治疗,可进展为呼吸衰竭。该病例中,临床药师对患者急性进展的肺部损伤的发生进行了评估、判断,并根据用药史进行关联性分析,判断很可能为rhG-CSF引起的嗜酸性粒细胞肺炎,同时协助医生制订治疗方案,促进了患者的成功救治。
Case analysis of acute eosinophilic pneumonia caused by recombinant human granulocyte stimulating factor (rhG-CSF)
doi: 10.12206/j.issn.1006-0111.202202029
- Received Date: 2022-02-14
- Rev Recd Date: 2022-06-30
- Available Online: 2022-07-27
- Publish Date: 2022-07-25
-
Key words:
- recombinant human granulocyte stimulating factor /
- drug-induced lung injury /
- eosinophilic pneumonia /
- adverse drug reaction
Abstract:
| Citation: | QU Runan, FAN Jialong, LIU Hui, ZHANG He, MAO Junqin. Case analysis of acute eosinophilic pneumonia caused by recombinant human granulocyte stimulating factor (rhG-CSF)[J]. Journal of Pharmaceutical Practice and Service, 2022, 40(4): 364-367. doi: 10.12206/j.issn.1006-0111.202202029 |







 DownLoad:
DownLoad: