-
全球每年由念珠菌引发的侵袭性真菌感染病例约有70万例[1],特别是在重症监护室中,患者由于免疫力低下,更易受到真菌感染所带来的危害。据报道,成年人感染念珠菌血症的死亡率高达40%~70%[2]。与此同时,白念珠菌(Candida albicans)作为临床最常见的机会致病性念珠菌,又是全球范围内侵袭性念珠菌的最主要病原体[1]。因此,针对白念珠菌感染的药物治疗研究,一直是人们关注的热点问题。目前,临床上广泛应用于治疗白念珠菌感染的抗真菌药物主要有唑类(氟康唑、伊曲康唑)、多烯类(两性霉素B)、棘白菌素类(卡泊芬净)和5-氟胞嘧啶。然而,随着临床上抗真菌药物的滥用,耐药菌株的报道也越来越多,严重影响了常规抗真菌药的疗效。更加不幸的是,近年来研究发现,即便是严格使用经体外药敏试验提示敏感的抗真菌药物进行治疗,仍有部分患者表现出迁延不愈和复发的症状,这种临床疗效与菌株低耐药性不一致的现象可能与白念珠菌药物耐受菌株的增加有关[3]。
耐受性是指药物敏感菌株在最低抑菌浓度(MIC)以上的高浓度药物中的生长能力,其特征是能够在高剂量抗真菌药物中存活而MIC不变。相反,耐药性则通常是由遗传突变引起的,其特征是测试菌株的 MIC升高[4]。临床菌株的抗真菌药物敏感性实验是在24 h读取的,但耐受菌株生长缓慢,在培养24~48 h后才会显现出高于MIC下生长的能力,因此,在临床检测中,真菌对药物的耐受性在很大程度上被忽视[3, 5]。然而,随着持续性念珠菌死亡率的增加,人们对菌株耐受性问题的关注也日益增多[6]。已有多项研究表明,临床分离株中有20%~60%的菌株表现出对药物的耐受性,进一步解释了临床菌株耐受性和感染治疗失败的关联[3, 5]。由此可见,白念珠菌的耐受问题给目前的临床治疗带来了更加严峻的挑战,积极应对真菌耐受性问题,开发相应的药物和治疗策略迫在眉睫。
小檗碱(BBR)又称黄连素,是一种分离自植物黄连根茎的天然季苄基异喹啉生物碱[7]。BBR临床上广泛运用于治疗胃肠炎,细菌性痢疾等肠道疾病,它的抗菌谱较广,在体外对多种革兰阳性及阴性细菌均具有抑菌作用,且具有安全性高,不良反应少的特点。据报道,BBR在其浓度为10~50 mg/L时具有一定的抗真菌作用[8]。课题组前期研究显示,BBR与氟康唑(FLC)联合使用具有显著的协同抗耐药真菌作用,通过本课题的进一步研究发现,BBR与FLC联合使用对FLC耐受白念珠菌也具有良好的抑制作用,为抗耐受真菌药物的研发提供了一定的实验基础。
-
白念珠菌实验株SC5314来自美国Georgetown大学。白念珠菌(C. albicans)临床株Y0109、9821、7879、7654、9296、9196、7781由海军军医大学第一附属医院及第二附属医院提供。
-
BBR(CAS号: 2086-83-1,货号:B875003-100 mg,纯度≥99%,购自Macklin公司); FLC(CAS号: 86386-73-4,货号:F830935-5g,纯度:98%,购自Macklin公司);二甲基亚砜(DMSO,购自国药集团化学试剂有限公司);酵母浸膏(购自BD公司);蛋白胨(购自BD公司);RPMI Medium 1640(购自Gibco公司);吗啉基丙磺酸(MOPS,购自Amresco公司);NaOH(购自Amresco公司)。
-
生物安全柜(BSC-1004II A2,苏州安泰空气技术有限公司);小型离心机(Hitachi CT15RE);生物显微镜(LW100T,北京测维光电技术有限公司);涡旋仪(Thermo vortex maxi mix Ⅱ);霉菌培养箱(MJ-150-Ⅰ,上海一恒科学仪器有限公司);酶标仪(Thermo Multiskan FC,赛默飞世尔上海仪器有限公司)。
-
YPD液体培养基:酵母浸膏10.0 g,蛋白胨20.0 g,加入800 ml超纯水,充分搅拌溶解后加入D-葡萄糖20.0 g,溶解后,继续加入超纯水定容至1 000 ml,经高压蒸汽灭菌(121℃,15 min)后,自然冷却至室温,密封放置于4℃冰箱保存[9]。YPD固体培养基:在YPD液体培养基成分的基础上加入20.0 g琼脂,高压蒸汽灭菌后,趁热倒入90 mm平皿中,晾干备用。
PBS缓冲溶液:精密称取NaCl 8.0 g,Na2HPO4·12H2O 3.57 g,KCl 0.2 g,KH2PO4 0.24 g,通过三蒸水充分溶解,并定容至1 000 ml,高温高压灭菌(121℃,15 min)后置于4℃冰箱内保存[9]。
RPMI
1640 培养基:RPMI Medium1640 10.0 g,NaHCO3 2.0 g,吗啉基丙磺酸34.5 g,加超纯水充分溶解后,定容至1 000 ml,加入NaOH适量,调pH值至7.0,经0.22 μm微孔滤膜过滤除菌,放置于冰箱4℃保存备用[9]。 -
菌株于YPD与甘油1∶1混合的溶液中保存,冻存于−80℃冰箱中。菌株活化时,吸取10 μl菌液加入装有1 ml 新鲜YPD培养液的15 ml玻璃摇菌管中,在30℃ 气浴恒温振荡培养箱中震荡(200 r/min)培养24 h,之后再次从菌悬液中吸取10 μl加入到1 ml新鲜YPD培养液中,继续以30℃震荡培养16 h后即活化完成,此时真菌处于指数生长的后期,可用于后续实验。
将活化完成的待测菌株转移至1.5 ml离心管中,以
3000 rpm离心1 min,吸弃上清液,随后使用1 ml PBS缓冲液反复吹打洗涤菌株,次离心弃上清液,如此反复3次后再用1 ml PBS缓冲液重悬菌液。取10 μl真菌原液稀释后使用细胞计数板于生物显微镜下计数,计算出真菌原液浓度,用RPMI 1640培养液稀释配制成实验所需菌液浓度。 -
MIC依据美国临床和实验室标准协会(CLSI)出版的微量液基稀释法实验手册(M27-A3)所规定的实验方法与试验标准来测定。具体方法如下:首先将处于指数生长末期的待测菌株用RPMI 1640培养基调整菌浓度至1×103 CFU/ml(菌落形成单位)。取一块96孔板,在第1列加入RPMI 1640培养基100 μl作为空白对照,在第2列加入菌液200 μl,第3~12列各加入菌液100 μl;随后于第2列各孔中加入提前配置好的FLC药液,吹打混匀后,吸出100 μl含药菌液加入到后一列各孔中,如此以2倍倍比稀释至第11列,第12列作为只含菌液的生长对照;并且保证每列至少做3个复孔,以减少实验误差。最后,将96孔板放置于30℃恒温箱中静置培养。培养24、48 h后,用酶标仪测定各孔在630 nm波长处的A值,其中A630刚好小于生长对照孔50%和80%所对应的药物浓度即为该菌FLC的MIC50和MIC80。
-
将活化好的待测菌株使用PBS缓冲液洗净重悬,并用PBS缓冲液将其稀释成浓度为1×106 CFU/ml的菌悬液,吸取100 μl菌液均匀涂布于YPD固体培养基中(考察协同作用时,培养基中应根据需求加入相应浓度的BBR)。随后,在培养基中每隔一定距离放置共7片灭菌滤纸片,在纸片上滴加等体积(5 μl)提前配制好的FLC药液,使滤纸片的载药量依次为0、0.78、1.56、3.125、6.25、12.5、25 μg,待药液吸收完全后将其倒置于30℃恒温培养箱中静置培养72 h,每24 h取出观察真菌生长状况并拍照记录。在筛选耐受菌时,在培养基正中间放入1片灭菌滤纸片,在纸片上滴加50 mg/ml的FLC药液5 μl,使纸片的载药量为250 μg,放置于30℃恒温培养箱中静置培养48 h,每24 h取出观察真菌生长状况并拍照记录[10]。
-
实验选取了8株白念珠菌(含7株临床株)测定其对FLC的MIC值(表1)。8株白念珠菌的MIC值均小于0.5 μg/ml,该结果表明,这8株白念珠菌皆为FLC敏感菌株。
菌株 MIC50(μg/ml) MIC80(μg/ml) SC5314 0.125 0.250 Y0109 0.250 0.500 9821 0.125 0.125 7879 0.125 0.125 7654 0.125 0.125 9296 0.250 0.250 9161 0.250 0.250 7781 0.125 0.125 -
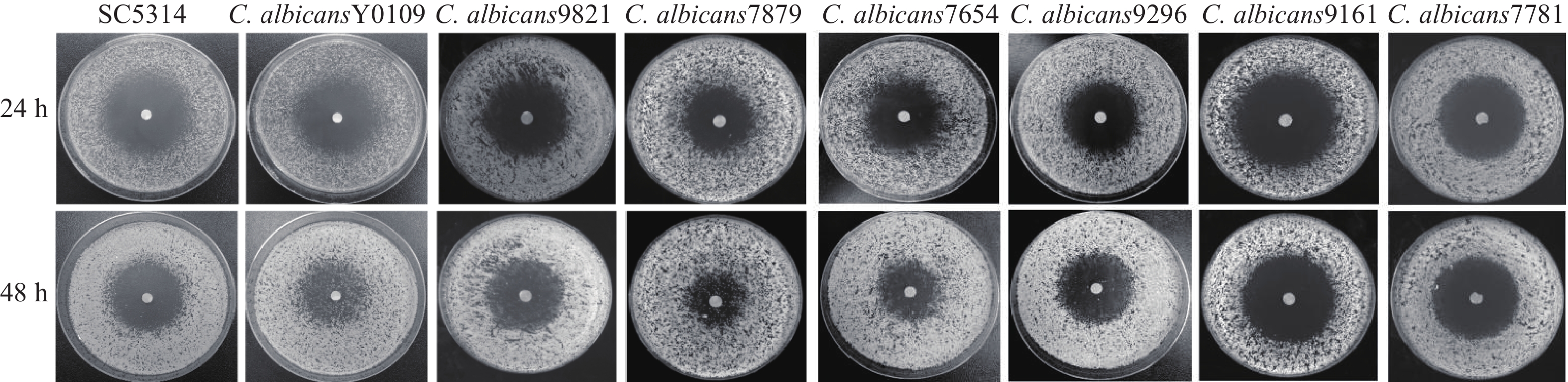
利用琼脂平皿纸片扩散实验,考察上述8株敏感型白念珠菌对FLC的耐受性。结果显示,在单用FLC的情况下,恒温培养24 h后,8株菌株均可观察到明显的抑菌圈,而培养48 h后,在菌株 Y0109、9821、7879、7654、9296的抑菌圈中,可以观察到明显的菌落生长,而其余菌株的抑菌圈内无菌落生长,该结果表明,菌株Y0109、9821、7879、7654、9296对FLC产生了耐受现象,可将其归类为FLC耐受菌株(图1)。
-
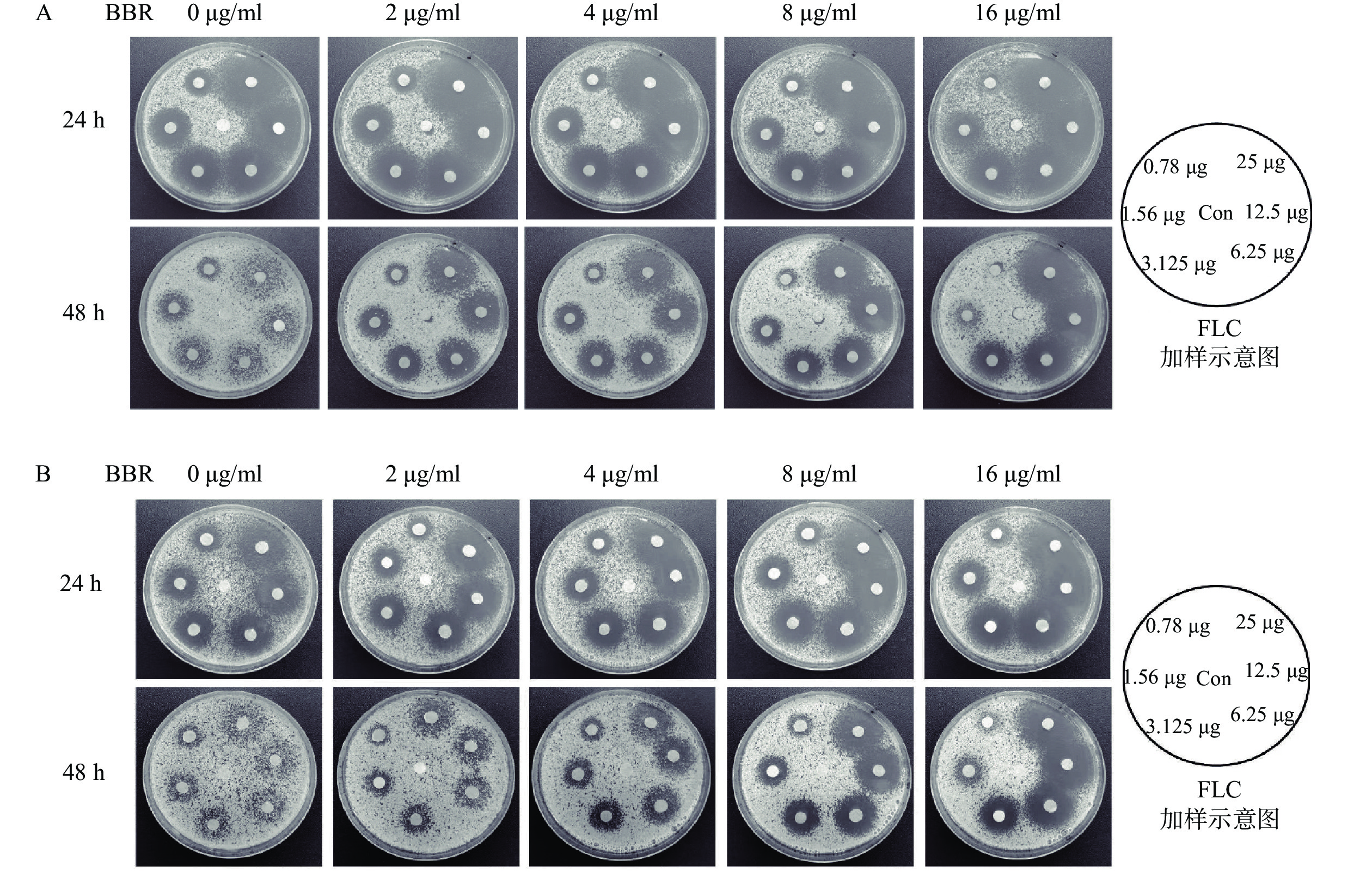
从考察菌株耐受性的抑菌圈实验中可以看出,5株氟康唑耐受菌株根据耐受强度可大致分为2类:高度耐受菌株Y0109、7879、7654;低度耐受菌株9821、9296。课题组从这2类中分别选择了Y0109及9821作为研究对象,利用琼脂平皿纸片扩散实验考察BBR与FLC联用是否具有抗FLC耐受白念珠菌作用。结果显示,耐受菌Y0109和9821在培养48 h后,与不含BBR的对照培养皿相比,含不同浓度(2~16 μg/ml)BBR平皿上的FLC载药滤纸片周围形成了明显的抑菌圈,抑菌圈内的菌落数随着BBR浓度的升高而逐渐减少,抑菌圈随BBR浓度的增加而逐渐清晰,随FLC载药量的增大而增大,显示出剂量依赖关系(图2)。上述结果表明,BBR与FLC联合用药具有良好的抗FLC耐受白念珠菌的作用。
-
白念珠菌对抗真菌药物的耐药问题一直是临床抗真菌感染研究的热点,而针对其耐受相关问题的研究却往往被人们忽视。多项研究表明,耐受是耐药的重要前提和基础,耐药突变更有可能源自于真菌的耐受亚群[3, 11-12]。因此,研究白念珠菌对抗真菌药物的耐受机制和相应的治疗策略具有重大的临床意义。
BBR作为一味历史悠久的抗菌药,在我国作为OTC药物用于防治腹泻性疾病已超过60年,其疗效和安全性均得到了普遍认可。本课题组前期研究发现,BBR与FLC在体外具有较好的协同抗FLC耐药白念珠菌的作用,这种协同作用与菌株对FLC的抗性有关,且两药的协同作用取决于BBR的浓度,而不是FLC的浓度[13]。进一步研究发现,FLC能够对细胞膜造成损伤,从而促进BBR对白念珠菌的侵袭,随后,BBR通过引起白念珠菌的细胞周期阻滞和DNA损伤发挥抗菌作用[14]。
目前,越来越多的研究表明,耐受和耐药的产生机制不同,而压力应答调控被认为是白念珠菌产生药物耐受的最重要方式之一。压力应答调控是真菌的一种应激策略,这一机制的产生对药物的靶点没有直接的影响[15]。它主要通过包括热休克蛋白90(Hsp 90)、蛋白激酶C、钙调磷酸酶以及雷帕霉素靶蛋白(TOR)等在内的关键因子与其相应的Ca2+-钙调磷酸酶、PKC-MAPK、Rim途径和HOG信号通路来调节白念珠菌对压力环境的应答,从而对唑类、多烯类和棘白菌素类等抗真菌药物产生耐受作用[16]。此外,白念珠菌还可以通过压力应答调控来影响其对药物的摄取和外排,从而间接地促进白念珠菌对药物的耐受能力[3]。在本研究中,我们发现BBR与FLC的联合用药对于FLC耐受白念珠菌具有很好的疗效,其作用机制是否与抑制白念珠菌的压力应答调控有关有待进一步探究。
联合用药一直以来都是临床抗真菌治疗的重要发展方向,该治疗策略不仅可以克服真菌的耐受与耐药难题,还可以增强原有药物的抗真菌作用,极大缓解新药研发的压力。本课题组研究发现,BBR与FLC联用不仅具有显著的协同抗FLC耐药白念珠菌作用,对FLC耐受白念珠菌也具有较强的抑制作用,为寻找新的抗耐药和耐受白念珠菌药物和治疗方法提供了新思路,值得我们进一步深入探索。
Study on the effect of berberine combined with fluconazole on fluconazole-tolerant Candida albcians strains
doi: 10.12206/j.issn.2097-2024.202409047
- Received Date: 2024-09-23
- Rev Recd Date: 2024-11-23
- Available Online: 2025-02-21
- Publish Date: 2025-02-25
-
Key words:
- Candida albicans /
- berberine /
- fluconazole /
- drug combination /
- drug tolerance
Abstract:
| Citation: | SONG Zecheng, MA Shanshan, HU Qiaoling, ZHONG Hua, WANG Yan. Study on the effect of berberine combined with fluconazole on fluconazole-tolerant Candida albcians strains[J]. Journal of Pharmaceutical Practice and Service, 2025, 43(2): 87-91. doi: 10.12206/j.issn.2097-2024.202409047 |







 DownLoad:
DownLoad: