-
外科手术部位感染(SSI)是医疗保健相关感染的常见原因[1],大多数SSI发生的平均时间为术后12 d[2]。耐甲氧西林金黄色葡萄球菌(MRSA)是指对已经批准的所有β内酰胺类抗菌药物有交叉耐药的金黄色葡萄球菌[3]。感染MRSA外科伤口较严重的患者,建议静脉输注糖肽类、利奈唑胺或达托霉素治疗[3]。因临床应用万古霉素经验丰富,为胃肠外首选[4]。但其治疗窗窄、不良反应多、血药浓度影响因素较多等特点,根据患者临床情况实施治疗药物监测(TDM)和个体化用药显得尤为重要。笔者介绍1例临床药师对足损伤术后感染MRSA患者进行药学监护的体会。
-
患者,男,17岁,体重60 kg,2020-05-04因“车祸致左足开放性外伤,出血30 min”入院,主要诊断为足部开放性损伤伴骨折、足部损伤、跟腱断裂。05-05行Ⅰ期清创+骨折切开复位内固定+跟腱修复+甲床修复术,术后头孢呋辛预防48 h。05-07手术切口感染,给予头孢呋辛治疗,05-08行Ⅱ期清创+创面封闭式负压引流术。05-11出现发热,体温最高38.2 ℃,炎性指标异常升高,换用万古霉素1.0 g ivgtt q12h。05-12切口分泌物培养+药敏示:MRSA、多重耐药,万古霉素敏感。05-19行Ⅲ期左足清创+带蒂皮瓣转移修复+跟腱修复术,头孢呋辛1.5 g ivgtt q8h预防感染,术后次日切口感染,体温最高38.7 ℃,换用万古霉素1.0 g ivgtt q12h抗感染治疗。其他治疗:Ⅰ~Ⅲ期术后常规氟比洛芬酯注射液镇痛3 d,Ⅲ期术后地塞米松抗炎、甘油果糖消肿、氟比洛芬酯注射液镇痛3 d,改为双氯芬酸钠胶囊。05-22万古霉素血药浓度检测为4.08 μg/ml,05-23调整万古霉素剂量为1.0 g ivgtt q8h,停用甘油果糖、地塞米松,05-26停用双氯芬酸钠胶囊。05-25、05-29复测万古霉素血药浓度为8.41和10.23μg/ml。在增加万古霉素剂量的次日上午,患者出现面部潮红症状,调慢滴速,症状缓解至消失,未再出现类似ADR。05-29出现急性肝损伤,停用万古霉素,给予甘草酸二铵保肝治疗1周,06-04切口恢复良好,准予出院。两周后随访,肝功能恢复正常。
-
术后第3天,患者发生足部切口感染,且为入院48 h后发生,予头孢呋辛治疗,体温、炎性指标未得到明显改善,临床药师高度怀疑为医院获得性MRSA。根据《哈里森感染病学》皮肤软组织感染治疗,对于社区或医院获得性金黄色葡萄球菌感染,对β-内酰胺类抗生素无应答,需换用抗MRSA药物治疗。临床药师建议换用万古霉素1.0 g ivgtt q12h治疗,医师采纳意见,当晚患者体温恢复正常。Ⅲ期手术预防用药,临床药师针对患者本次住院已检出MRSA,且近半年骨科MRSA检出率为62.5%,建议调整为万古霉素[5],但医师未采纳药师建议。
-
术后第3天,出现切口红肿热痛、大量渗出、发热,诊断外科切口感染明确,选择万古霉素。临床药师根据未接受血液透析的成人胃肠外万古霉素剂量推荐表[6],结合患者体重、非重症感染、肌酐清除率指标,推荐初始剂量为1.0 g ivgtt q12 h。
-
患者05-29因出现急性肝损伤,根据《万古霉素临床应用专家共识》[4]推荐疗程为7~14 d,患者用药9 d,临床药师根据患者临床症状无明显红肿热痛,炎性指标趋于正常,可停用抗菌药物治疗。
-
05-19行Ⅲ期术后次日,切口出现感染征象,给予万古霉素抗感染治疗。05-20至05-23患者切口感染部位症状缓解不明显,一直低热状态。临床药师建议行万古霉素血药浓度监测,同时建议停用可能影响万古霉素血药浓度的甘油果糖,并参考《万古霉素个体化给药临床药师指引》[7]调整其剂量为1.0 g ivgtt q8 h。万古霉素剂量调整前血药浓度为4.08 μg/ml,调整后复测2次血药浓度分别为8.41、10.23 μg/ml。通过停用甘油果糖、TDM、调整万古霉素剂量,患者血药浓度显著升高,并达到有效治疗浓度[4]。
影响成年患者体内万古霉素的浓度因素包括年龄、中重度外周水肿、肾功能异常、肥胖及肾功能亢进等因素[8-9]。患者术后切口部位严重水肿,炎性反应明显,在一定程度上会对血液内稳态产生一定影响,导致机体代谢药物的能力也受到一定影响。万古霉素联合应用甘油果糖可能会严重影响其血药浓度,有研究显示[10],渗透性药物能促进万古霉素在体内的清除和排泄,令血药浓度降低。本例患者本身存在严重组织水肿,同时使用渗透性药物甘油果糖,可能是影响万古霉素血药浓度过低的原因。肾功能亢进的原因包括烧伤、粒细胞缺乏伴发热、脓毒血症、创伤、蛛网膜下隙出血等[11]。该患者严重创伤入院,肌酐清除率为145.94 ml/min,存在肾功能亢进,可能在一定程度上导致患者万古霉素血药浓度过低。
-
患者增加万古霉素使用剂量至1.0 g ivgtt q8 h,次日上午出现面部、颈部微潮红。临床药师结合患者用药史,采用诺氏评估量表评价ADR关联性,评分为7分,考虑很可能为万古霉素相关性引起的红人综合征(RMS)。RMS是在万古霉素输注期间或输注结束后立即出现的潮红,由组胺介导。组胺释放量一般与输注万古霉素的剂量和输注速度有关[12]。该患者在未调整万古霉素剂量之前,输注时间控制在60 min左右,一直未发生相关不良反应。临床药师建议先以给药速率≤10 mg/min输注(或1.0 g,输注时间≥100 min)[12],并密切监护。结果减慢滴速后,患者潮红症状消退,并未再出现RMS症状。
-
对于肾功能正常,合并肾损伤药物且疗程较长的患者,应密切监测肾功能[4]。本例患者在Ⅰ~Ⅲ期术后,常规使用非甾体类药物镇痛,为避免增加肾损伤可能性,结合患者疼痛评分3分,临床药师建议尽早停用非甾体类药物,或换用肾功能损伤最小的阿片类镇痛药[13],医师采纳该意见。
-
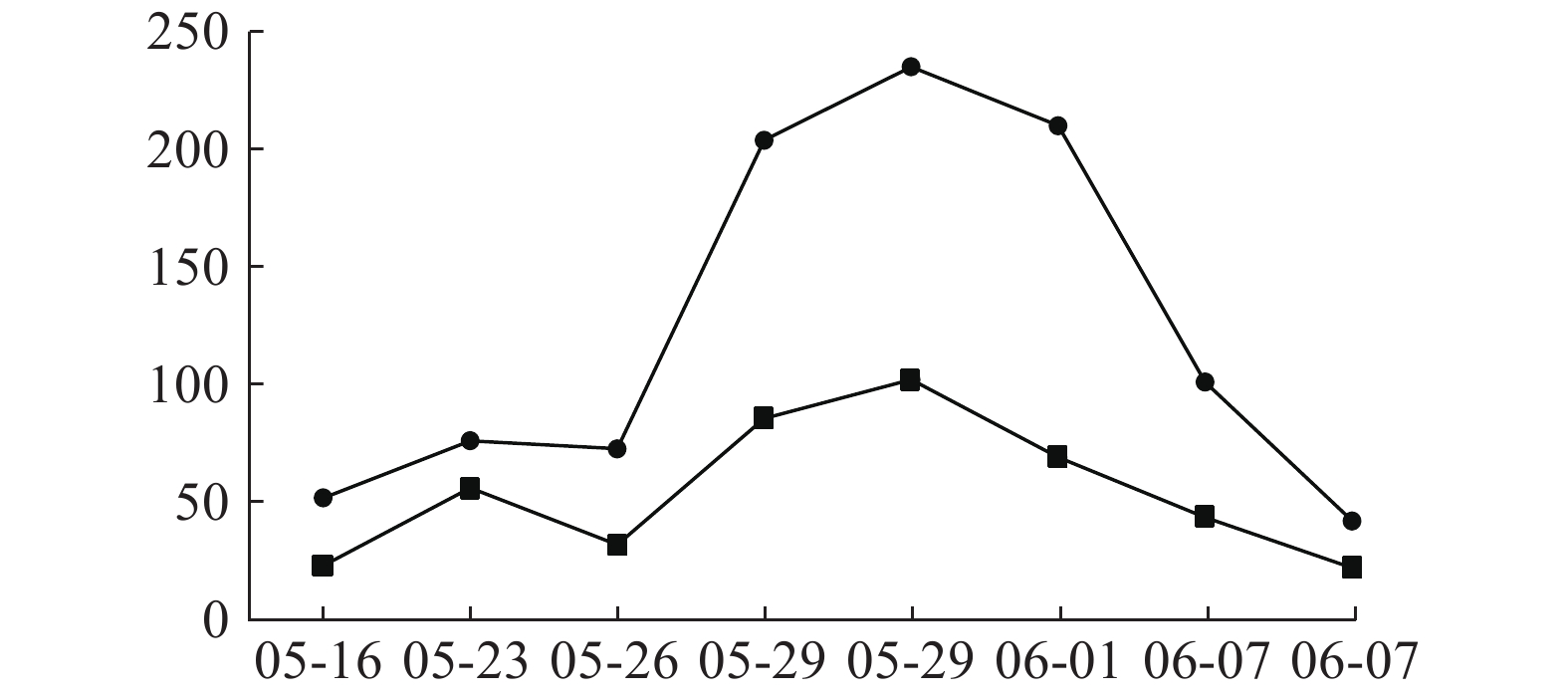
患者入院时肝功能正常,05-09开始用万古霉素1.0 g ivgtt q12 h治疗,05-16查肝功示ALT 51.7 U/L,05-18停用;05-20因病情需要再次使用万古霉素1.0 g ivgtt q12 h治疗,05-23调整剂量为1.0 g ivgtt q8 h。05-26复查肝功示ALT 72.6.00 U/L,AST 31.8 U/L,出现转氨酶进行性小幅升高,继续万古霉素抗MRSA治疗,符合《EASL:药物性肝损伤的临床实践指南》[14]。05-29两次复查肝功示:ALT 203.8 U/L,AST 85.5 U/L;ALT 235.00 U/L,AST 102.00 U/L,提示ALT≥3倍正常值上限,出现急性肝损伤,停用万古霉素,给予甘草酸二铵保肝治疗,06-04出院并停用甘草酸二铵。06-25随访肝功能完全恢复正常。万古霉素治疗前后ALT、AST指标变化见图1。
临床药师以诺氏评估量表作ADR关联性评价,评分为9分,患者肝损害与万古霉素不良反应发生有时间上的关联,高度可能为万古霉素引起肝功能损伤。万古霉素导致肝损伤报道例数较少[15-18],以血清转氨酶升高为主[15-18],临床表现可为无症状性肝损伤或急性肝损伤。本例患者系无症状性急性肝损伤,提示关注万古霉素长疗程治疗中肝损伤ADR。
-
临床药师作为医疗团队中的一员,在药物使用过程中,尤其在药物浓度监测和药学监护方面发挥了重要作用。在该患者治疗过程中,临床药师查阅指南、文献及药品说明书,协助医师做好抗感染治疗方案的制定,并结合临床疗效,加强抗感染治疗的药学监护,分析治疗效果不佳原因,并有针对性地提出建议与改进措施,包括调整合并用药及药物剂量,避免和减少了万古霉素相关的RMS、肝肾功能损伤不良反应对患者进一步伤害,使患者临床获益更多。
The pharmaceutical care by clinical pharmacists for a foot injury patient with postoperative MRSA infection
-
摘要:
目的 探讨临床药师在术后感染MRSA患者药物治疗监护中作用。 方法 通过参与制订抗感染治疗方案、选择抗菌药物、识别MRSA感染高危因素、评估万古霉素疗效、利用TDM技术调整剂量,以及对万古霉素不良反应监护及处理。 结果 在临床药师的药学监护下,患者得到有效治疗,避免了万古霉素相关不良反应的进一步伤害。 结论 临床药师在促进患者及时康复、精准安全用药中发挥了重要作用。 -
关键词:
- 临床药师 /
- 万古霉素 /
- 耐甲氧西林金黄色葡萄球菌 /
- 药学监护
Abstract:Objective To explore the clinical pharmacist’s role in drug therapy and monitoring for the patient with postoperative MRSA infection. Methods Clinical pharmacists participated in planning anti-infective treatment, antimicrobial medication selection, identification of high-risk factors for MRSA infection, evaluation of vancomycin efficacy, dosage adjustment using TDM technology, monitoring and management of vancomycin adverse reactions. Results With the pharmaceutical care provided by clinical pharmacists, the patient received effective treatment with minimal vancomycin-related adverse reactions. Conclusion Clinical pharmacists played an important role in accelerating patient recovery by rational and safe medication use. -
Key words:
- clinical pharmacist /
- vancomycin /
- MRSA /
- pharmaceutical care
-
雀梅藤Sageretia thea(Osbeck)Johnst又名雀梅刺、对角刺、碎米子等,为鼠李科雀梅藤属植物,主要分布地区包括云南、安徽、江苏等[1-2]。根、茎、叶均可入药,其性甘、淡、平,具有降气化痰、祛风利湿等功效[3]。民间常用雀梅藤药材煎汤或浸酒内服治疗乳腺肿瘤、淋巴结肿大和水肿等疾病,具有较好效果[4]。现代药理研究表明,雀梅藤具有抗结直肠癌、抗炎、抗氧化、抗病毒、抗菌和肝保护等活性[5-6],但尚未见雀梅藤对乳腺癌等其他肿瘤影响的报道。该研究通过多种体外实验观察雀梅藤对乳腺癌细胞增殖及凋亡的影响,并初步探索其作用机制,以证实民间应用该药材治疗乳腺肿瘤的合理性,为进一步的药物开发奠定基础。
1. 材料和仪器
1.1 试剂和仪器
CCK8 试剂盒(大连美仑生物技术有限公司);Spark酶标仪(瑞士Tecan公司);二氧化碳培养箱(Thermo Fisher);96孔培养板(泰坦);电子分析天平(塞多利斯 BSA2245-CW);细胞计数仪(Corning 6749);倒置相差显微镜(奥林巴斯 IX73)。
1.2 药材提取
雀梅藤药材购自昆明井田药业有限公司,生产许可证号:滇20160155。经海军军医大学药学系生药学教研室辛海量教授鉴定为鼠李科雀梅藤属植物雀梅藤Sageretia thea(Osbeck)Johnst.的茎。取雀梅藤干燥药材660 g,粉碎后用8倍量75%乙醇回流提取3次,每次1.5 h。合并提取液,过滤后回收溶剂,得乙醇提取物。乙醇提取物用水溶解混悬,加入等体积的石油醚萃取3次,收集萃取液,通过旋转蒸发得到石油醚萃取部位。进一步采用真空冷冻干燥机在−80 ℃下冻干,分别称重,获得乙醇和石油醚提取物质量为57 g和0.91 g,提取得率分别为8.63%和0.13%。
1.3 提取物溶解
称取20 mg雀梅藤石油醚提取物溶于1 ml的DMSO溶剂中,然后用培养液稀释成不同药物浓度,药物最高剂量下的DMSO浓度不超过0.3%。同时,对照组培养液中添加0.3%的DMSO作为阴性对照。
1.4 细胞株
三阴性人乳腺癌细胞株MDA-MB-231、BT549购自中国科学院上海细胞库;人脐静脉血管内皮细胞株购自上海赋望实业有限公司。
2. 方法
2.1 细胞活力分析
分别取对数生长期的人三阴性乳腺癌细胞株MDA-MB-231和BT549及人脐静脉血管内皮细胞株(HUVEC)并计数,以每孔5×103个的细胞密度接种到96孔板,在37 ℃的细胞培养箱中过夜培养至细胞贴壁。实验分为对照组和给药组,对照组以正常培养基培养,给药组以不同浓度含药培养基孵育细胞24 h。随后按试剂盒说明书进行操作,每孔加入10%的CCK8试剂,在培养箱中孵育2 h后,用酶标仪在450 nm处检测各孔的吸光度(OD)值。对照组细胞活力换算为100%,其余各给药组按以下公式计算:细胞增殖抑制率(%)=[(对照组A值−实验组A值)/(对照组A值−空白组A值)]×100%。
2.2 平板克隆试验
取上述对数生长期的人三阴性乳腺癌细胞株,以每孔500个细胞的密度均匀接种在12孔板内,过夜,使细胞贴壁,随后加入雀梅藤提取物孵育24 h。吸弃培养基,用含10%的胎牛血清培养基继续培养,当培养皿中出现肉眼可见的克隆形成时,终止培养。吸弃上清液,用PBS小心浸洗,然后甲醇固定。去除固定液,加入适量的结晶紫染色液进行染色,采用PBS多次轻轻洗去周边染色液,干燥后拍照,随后用Image J软件进行统计分析。
2.3 活死细胞分析
将两种乳腺癌细胞接种于96孔板,放置培养箱中过夜,随后加入提取物孵育24 h。吸弃培养基,用PBS温和洗涤细胞一次,每孔加入100 μl的Calcein AM/PI染色工作液,放入37 ℃培养箱中避光孵育15 min后,用高内涵系统采集图像。
2.4 细胞周期分析
取对数生长期乳腺癌细胞株,以每孔40万个细胞接种于6孔板,培养箱中过夜,待细胞贴壁后,用含不同浓度提取物的培养基处理24 h,消化,离心收集细胞,以预冷的70%乙醇混悬固定过夜。离心,去除乙醇,用PBS清洗一次,加入500 μl的碘化丙啶染色工作液,避光染色30 min后用流式细胞仪分析细胞周期。
2.5 流式凋亡分析
将对数生长期的三阴性乳腺癌细胞株以每孔40万个接种于6孔板中,过夜,待细胞贴壁后,用含不同浓度提取物的培养基孵育24 h。消化,离心收集细胞,用100 μl的1×结合缓冲液混悬后加入FITC Annexin V 和PI各5 μl,轻微振荡,室温下避光孵育15 min,流式细胞仪分析凋亡率。
2.6 DAPI染色分析
将上述对数生长期的人三阴性乳腺癌细胞株以每孔20万个接种于6孔板,过夜,待细胞贴壁后,用含不同浓度提取物的培养基孵育24 h,吸弃培养基,每孔加入1 ml稀释过的DAPI染液孵育细胞10 min,PBS清洗2遍后采用Cytation 5拍照。
2.7 线粒体膜电位(MMP)分析
将对数生长期的人三阴性乳腺癌细胞株以每孔20万个接种于6孔板,过夜,待细胞贴壁后,用含不同浓度提取物的培养基孵育细胞24 h。吸弃培养液,PBS洗涤细胞之后每孔加入1 ml的JC-1染液,在37 ℃培养箱中孵育20 min。吸除上清液,用缓冲液洗涤细胞3次后加入2 ml细胞培养液,高内涵系统拍照。
2.8 活性氧(ROS)含量检测
取上述对数生长期细胞株,以每孔20万个的细胞密度接种于6孔板,过夜,待细胞贴壁后,用含不同浓度提取物的培养基孵育24 h。吸弃培养基,每孔加入1 ml含DCFH-DA的新鲜培养基孵育细胞20~30 min,DAPI复染,采用高内涵系统拍照。
2.9 统计学处理
使用Graphpad Prism 8.0.1分析软件对所获得的实验数据进行统计学分析,组间比较采用单因素方差分析,两组比较采用t检验,以P<0.05为差异有统计学意义。
3. 结果
3.1 抑制乳腺癌细胞生长
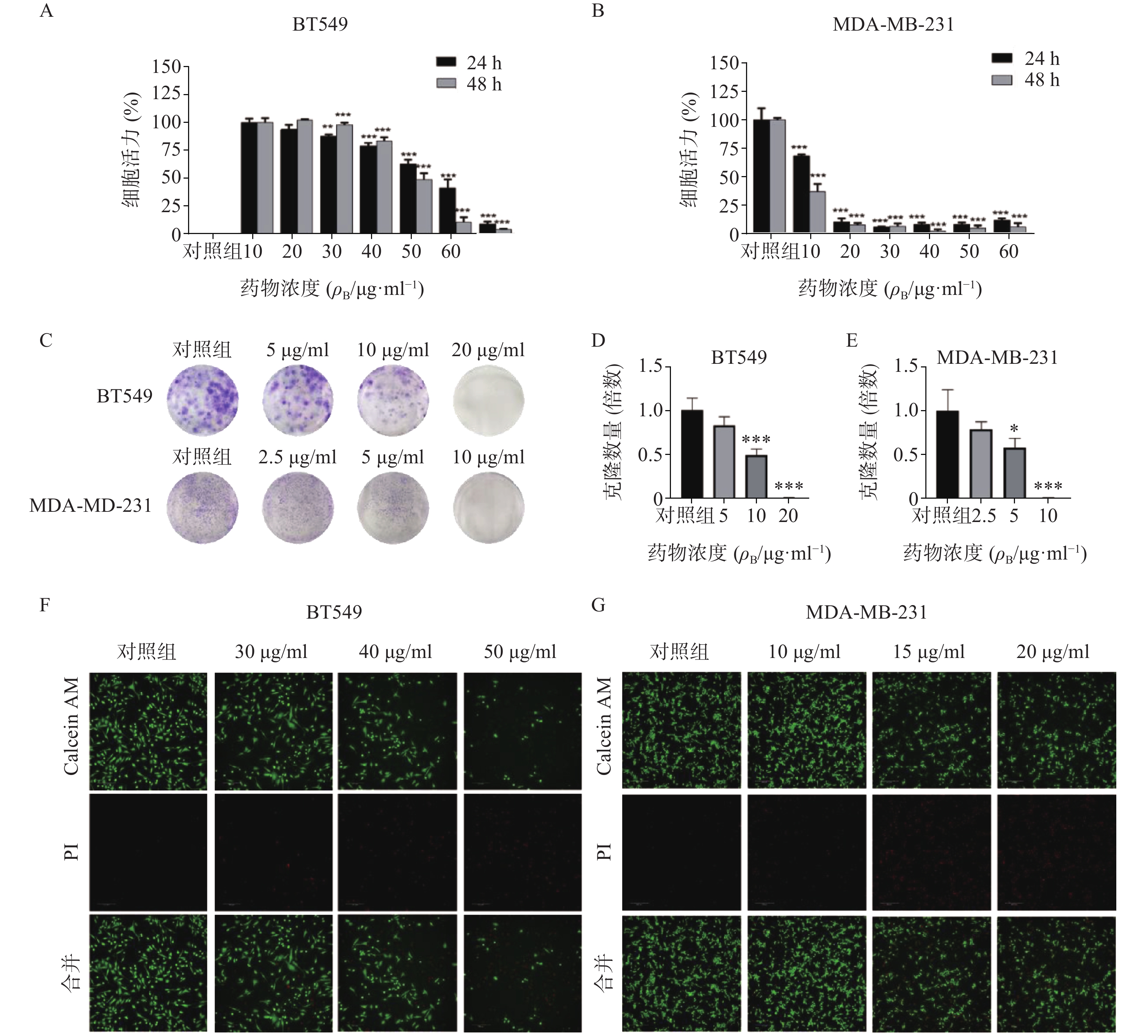
通过细胞活力分析发现,雀梅藤石油醚提取部位对多种癌细胞均有明显细胞毒性,其中对乳腺癌细胞株抑制作用最强,而且明显强于乙醇提取物。结合临床应用,实验选择两种人三阴性乳腺癌系(BT549和MDA-MB-231)进一步研究(见图1)。CCK8结果表明(图1A-B),雀梅藤石油醚提取物以剂量和时间依赖的方式抑制乳腺癌细胞活力,作用24 h和48 h的IC50值分别为45.40、12.23 μg/ml和38.87、7.60 μg/ml。平板克隆实验结果显示(图1C-E),随着雀梅藤石油醚提取物剂量的增加,两种乳腺癌细胞生长均被显著抑制。浓度分别在10 μg/ml和20 μg/ml时,MDA-MA-231和BT549细胞株的生长被完全抑制。Calcein AM/PI活死细胞染色显示(图1F-G),随着药物剂量增加,活细胞(绿色)数量较对照组显著减少,而死亡细胞(红色)数量则显著增加,与对照组比较有极显著差异。
3.2 诱导乳腺癌细胞周期阻滞
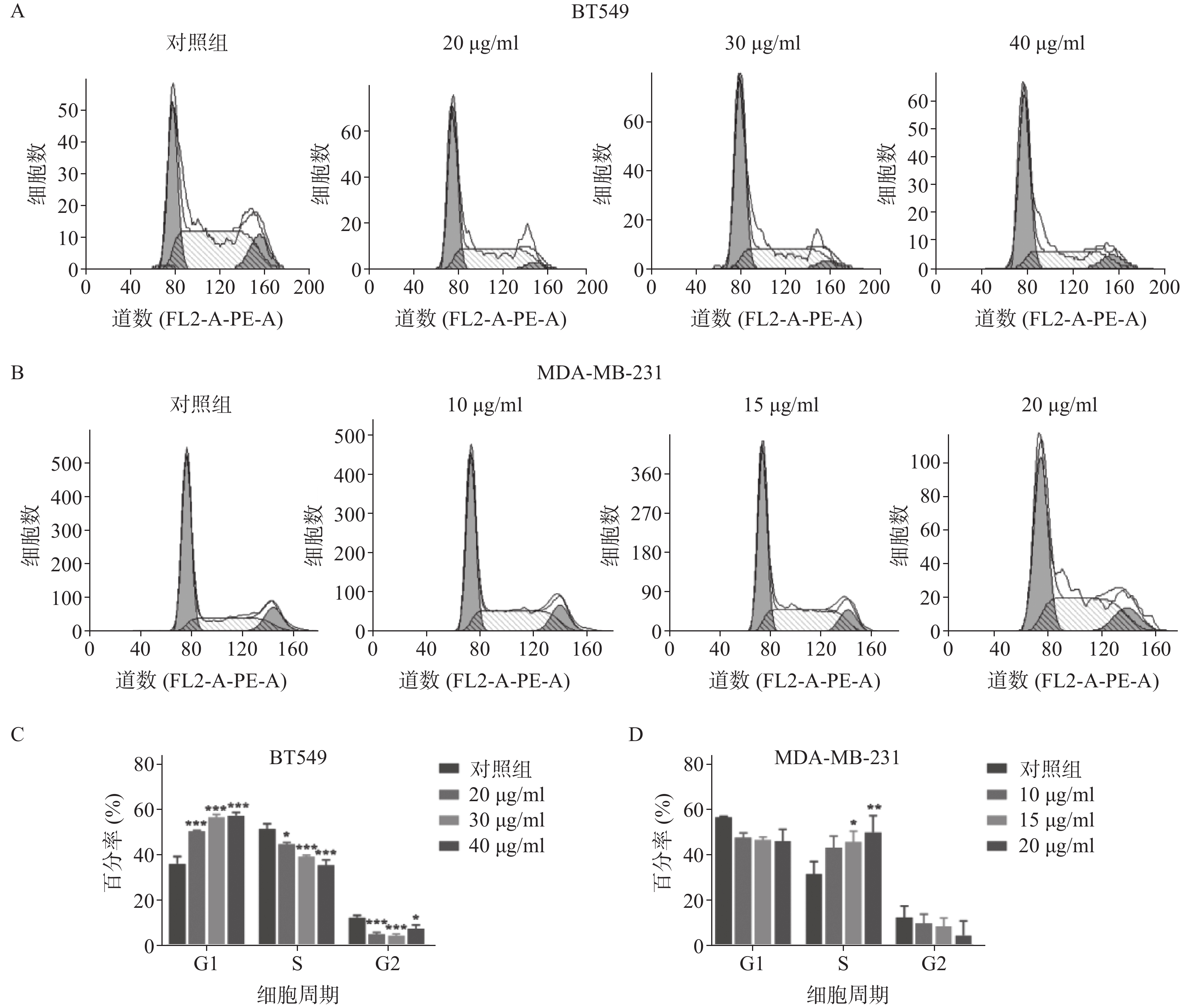
雀梅藤石油醚提取物孵育乳腺癌细胞24 h后,采用流式细胞仪测定细胞的增殖周期情况(见图2)。结果显示,药物明显阻滞两种乳腺癌细胞株的细胞周期,但对两种细胞阻滞周期不同,BT549细胞阻滞在G1期(图2A和2C,给药组G1期细胞比率较对照组显著升高),MDA-MA-231细胞阻滞在S期(图2B和2D,给药组S期细胞比率较对照组显著升高),提示石油醚提取物对两种细胞株的细胞周期阻滞可能存在不同机制。
3.3 诱导乳腺癌细胞凋亡
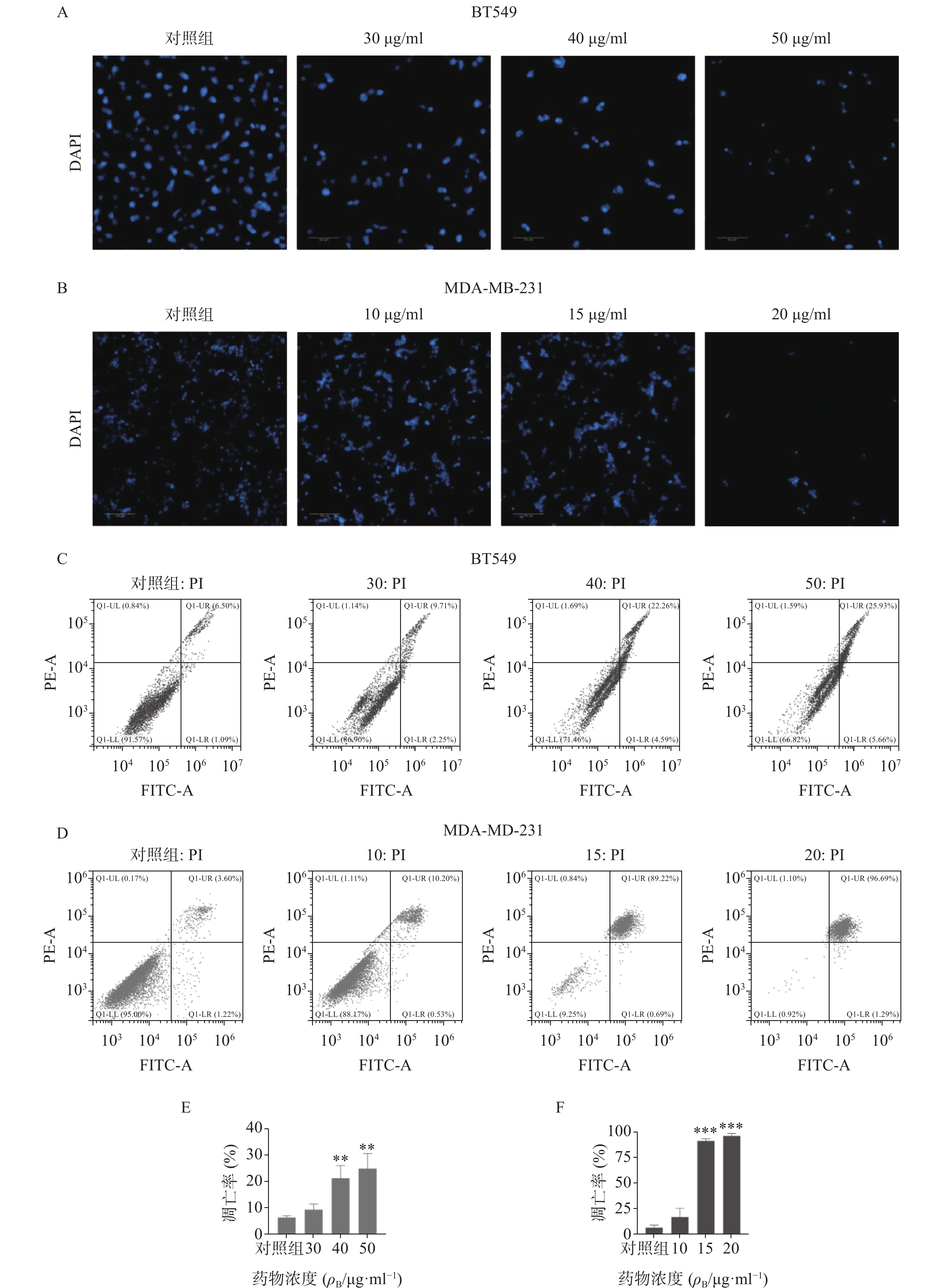
采用DAPI染色方法对细胞核形态进行分析(见图3)。如图3A-B所示,正常对照组乳腺癌细胞核呈均匀的圆形浅蓝色,药物处理后细胞核质固缩或碎裂成凋亡小体,且呈剂量依赖性。流式细胞仪凋亡定量分析显示(图3C-F),石油醚提取物显著增加两种乳腺癌细胞的凋亡率,与对照组比较有显著性差异,其中尤以MDA-MA-231细胞株明显,20 μg/ml浓度下几乎诱导细胞全部凋亡。
3.4 诱导线粒体膜电位坍塌
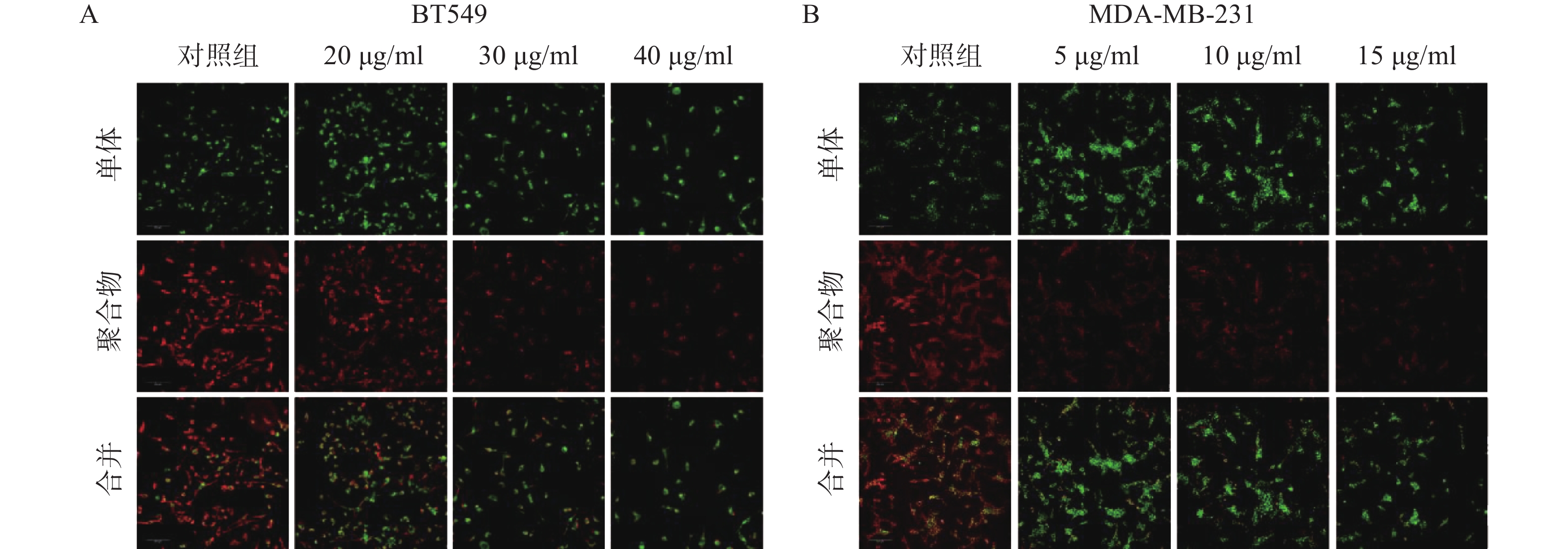
线粒体通路是肿瘤细胞最常见的凋亡途径,最典型的特征是线粒体膜电位(MMP)水平显著下降。因此,研究采用JC-1免疫荧光染色检测线粒体膜电位水平。结果如图4所示,给药组红色荧光随剂量增加明显减弱,绿色荧光则明显增强,说明给药组线粒体膜电位显著下降。实验结果提示,雀梅藤石油醚提取物可能通过损伤线粒体而促进了乳腺癌细胞凋亡。
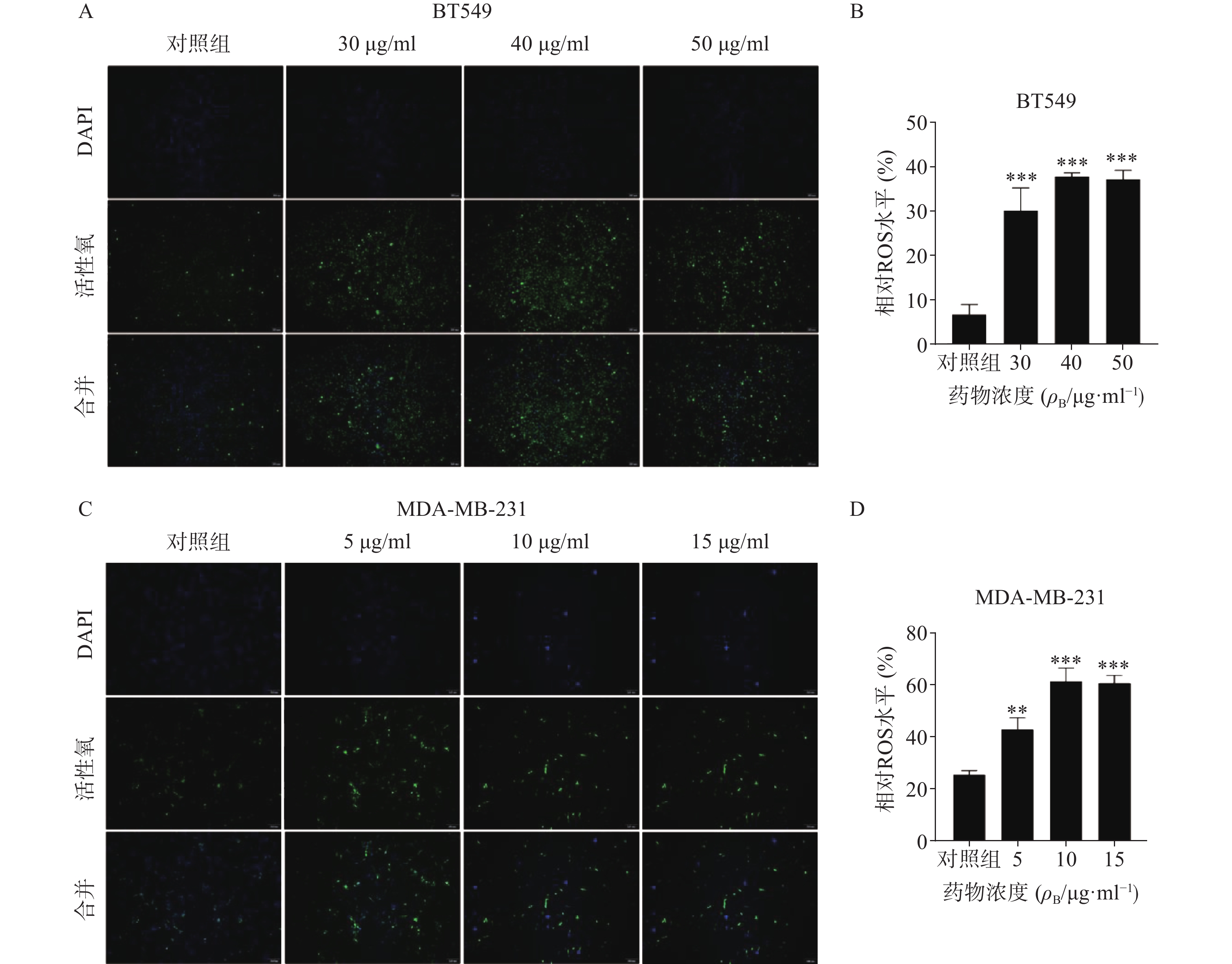
3.5 促进乳腺癌细胞活性氧生成
ROS升高是激活线粒体通路诱导肿瘤细胞凋亡的重要原因之一,因此进一步检测了药物处理24 h后ROS含量变化(图5)。结果代表ROS水平的绿色荧光在对照组仅有少量表达,而在给药组则显著增加,经统计学处理有显著性差异,其中尤以BT549细胞株明显,提示药物可能通过促进ROS生成而诱导了乳腺癌细胞凋亡。
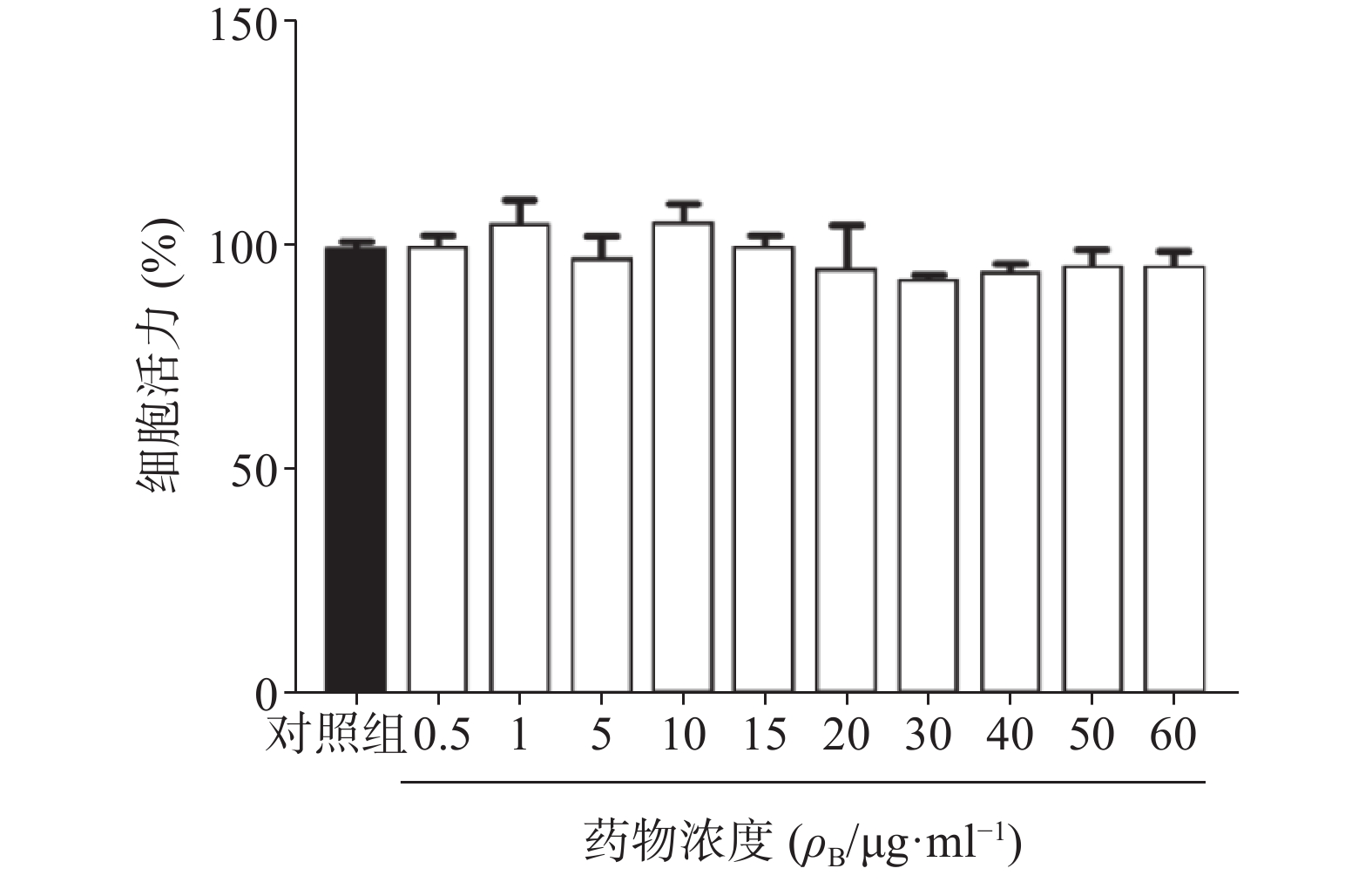
3.6 对正常血管内皮细胞活力的影响
为了确定雀梅藤提取物是否对正常细胞产生毒性,进一步采用同样剂量对人正常脐静脉血管内皮细胞(HUVEC)进行CCK8细胞活力分析。结果提取物孵育24 h后,即使在60 μg/ml的最高浓度下亦未观察到内皮细胞活力受到影响,与对照组比较无明显差异(图6),提示雀梅藤石油醚提取物对正常细胞并不产生毒性,具有较好的安全性。
4. 讨论
雀梅藤为云南等地民间常用中药,临床观察发现其对乳腺瘤生长有明显抑制作用[7],且毒性较小[4, 8]。研究前期对雀梅藤的乙醇、石油醚、乙酸乙酯、二氯甲烷、正丁醇等5个部位提取物进行了多种肿瘤细胞活性筛选,结果显示,对多数癌细胞,如乳腺癌、结肠癌、肝癌等,都具有明显杀伤作用,其中以石油醚部位提取物对癌细胞作用最为显著。进一步实验发现,雀梅藤石油醚提取物时间和剂量依赖地抑制乳腺癌细胞活力,显著减少细胞克隆形成率,阻滞细胞周期在G1/S期,明显增加癌细胞凋亡率,但并不影响正常血管内皮细胞活力,提示其细胞毒性具有明显的选择性。
引起细胞凋亡的途径包括线粒体通路、死亡受体通路和内质网应激通路,其中线粒体通路是药物诱导肿瘤细胞凋亡的最常见途径[9],因此研究人员进一步观察了雀梅藤石油醚提取物是否通过损伤线粒体诱导乳腺癌细胞凋亡。结果通过JC-1染色发现,两种乳腺癌细胞的线粒体膜电位均显著降低,提示雀梅藤提取物诱导了细胞线粒体途径的凋亡。
ROS的主要来源之一是线粒体内膜的呼吸链底物端,ROS升高会引起线粒体内膜损伤,造成细胞毒性,从而促进肿瘤细胞凋亡[10]。研究人员用荧光探针方法检测雀梅藤石油醚提取物孵育BT549和MDA-MB-231细胞后的ROS水平,结果发现代表ROS的绿色荧光逐渐增强,表明石油醚提取物显著升高了线粒体内ROS水平。这些结果提示,石油醚提取物可能通过升高线粒体内ROS水平,造成ROS累积,损伤了线粒体,导致线粒体内容物如细胞色素c等流出到细胞质,进而激活caspase级联瀑布反应,从而诱导了细胞凋亡[9,11]。
虽然雀梅藤提取物在体外研究中表现出较好的抗乳腺癌细胞生长作用,但是凋亡信号转导通路和作用靶点尚不明确,线粒体中蛋白表达的变化犹未可知,因此具体作用机制尚需进一步研究。此外,已有研究人员从雀梅藤药材中鉴定出43种化学成分,可分为有机酸类、黄酮类及其他类,有机酸类包括儿茶素及其衍生物等,黄酮类包括异槲皮素等[12]。但是雀梅藤提取物中究竟何种成分发挥主要抗癌作用仍需进一步证实。
-
[1] BERRÍOS-TORRES S I, UMSCHEID C A, BRATZLER D W, et al. Centers for Disease Control and Prevention Guideline for the Prevention of Surgical Site Infection, 2017[J]. JAMA Surg,2017,152(8):784-791. doi: 10.1001/jamasurg.2017.0904 [2] 巴特利特, 奥威特, 等. ABX指南: 感染性疾病的诊断与治疗[M]. 北京: 科学技术文献出版社, 2012 [3] 葛瑛. 《耐甲氧西林金黄色葡萄球菌感染防治专家共识》解读[J]. 中国临床医生, 2014, 42(3):11-12. [4] 万古霉素临床应用中国专家共识(2011版)[J]. 中国新药与临床杂志, 2011, 30(8): 561-573 [5] BRATZLER D W, DELLINGER E P, OLSEN K M, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery[J]. Am J Health Syst Pharm,2013,70(3):195-283. doi: 10.2146/ajhp120568 [6] RYBAK M J, LE J, LODISE T P, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists[J]. Am J Health Syst Pharm,2020,77(11):835-864. doi: 10.1093/ajhp/zxaa036 [7] 何志超, 伍俊妍, 邱凯锋. 万古霉素个体化给药临床药师指引[J]. 今日药学, 2015, 25(2):78-82. [8] ÁLVAREZ R, LÓPEZ CORTÉS L E, MOLINA J, et al. Optimizing the clinical use of vancomycin[J]. Antimicrob Agents Chemother,2016,60(5):2601-2609. doi: 10.1128/AAC.03147-14 [9] 唐莲, 严晓薇, 彭秋菊, 等. 肾功能亢进患者万古霉素血药浓度监测与临床疗效分析[J]. 中国医院药学杂志, 2018, 38(15):1629-1632. [10] 王凌, 眭玉霞. 渗透性治疗对神经危重症患者万古霉素血药浓度的影响[J]. 中国执业药师, 2016, 13(010):3-5. [11] HOBBS A L, SHEA K M, ROBERTS K M, et al. Implications of augmented renal clearance on drug dosing in critically ill patients: a focus on antibiotics[J]. Pharmacotherapy,2015,35(11):1063-1075. doi: 10.1002/phar.1653 [12] HEALY D P, SAHAI J V, FULLER S H, et al. Vancomycin-induced histamine release and "red man syndrome": comparison of 1- and 2-hour infusions[J]. Antimicrob Agents Chemother,1990,34(4):550-554. doi: 10.1128/AAC.34.4.550 [13] 广东省药学会. 临床药师术后疼痛管理指引[J]. 今日药学, 2019, 29(4):217-227. [14] European Association for the Study of the Liver. Clinical Practice Guidelines: Drug-induced liver injury. J Hepatol, 2019, 70(6): 1222-1261. [15] 周红玲, 刘年开, 丁楠. 万古霉素致严重肝损害1例[J]. 中国执业药师, 2012, 9(10):40-41. [16] 梁瑜, 孟真, 仓怀芹, 等. 注射用盐酸万古霉素致急性药物性肝损伤1例分析[J/OL]. 中国药物警戒, (2020-12-28) [2021-05-12]. http://kns.cnki.net/kcms/detail/11.5219.R.20201228.1229.002.html [17] SERRANTI D, MONTAGNANI C, INDOLFI G, et al. Antibiotic induced liver injury: what about children? J Chemother,2013,25(5):255-272. doi: 10.1179/1973947813Y.0000000090 [18] CADLE R M, MANSOURI M D, DAROUICHE R O. Vancomycin-induced elevation of liver enzyme levels[J]. Ann Pharmacother,2006,40(6):1186-1189. doi: 10.1345/aph.1G668 -





 下载:
下载:
 下载:
下载:


