-
化脓性血栓性静脉炎(STP)是指伴有细菌或真菌感染的血管内血栓形成[1],属于复杂性导管相关性血流感染并可引起局部或远处感染性并发症,在其治疗过程中抗菌药物的选择及使用具有关键作用[2]。此外,对于STP的抗凝治疗目前尚无统一认识,不同的医生选择也不尽相同[3]。STP虽不常见,但如果治疗不及时,会导致极高死亡率。本文从1例STP继发肺部感染患者的治疗过程,探讨合理抗感染及联合抗凝的必要性,并分析临床药师在重症医疗团队中开展药学监护的作用。
-
患者,男,17岁,身高165cm,体重65kg。2天前无明显诱因出现右下腹痛,伴恶心、呕吐,呕吐物为胃内容物,凌晨腹痛、呕吐加重,不能耐受,急诊至我院。实验室检查:白细胞(WBC) 6.41×109/L,中性粒细胞比率(N%) 84.1 %,C反应蛋白(CRP) 222.8 mg/L,降钙素原(PCT) 7.2 ng/ml,D-二聚体 9.17 mg/L,血肌酐(Scr) 114.1 μmol/L。影像学检查:腹部CT见少量腹水,大网膜及肠系膜增厚肿胀,盲肠及阑尾区域混杂密度占位,周围小淋巴结显示需排除阑尾炎伴周围脓肿。急诊以“急性化脓性阑尾炎”收治入院。患者先天性唐氏综合征,无其他特殊个人史及家族史。患者入院后病情进展迅速,出现呼吸、循环不稳定,肾脏损伤,经积极扩容补液后血压仍需大剂量去甲肾上腺素维持。急性生理与慢性健康评分(APACHE II)为14分,序贯器官衰竭检测评分(SOFA)为12分。
入院检查:腹膨隆,腹壁硬,全腹压痛,有肌紧张及反跳痛。体温38.2 ℃,心率160次/min,血压110/67 mmHg(去甲肾上腺素1.09 μg/kg·min),呼吸22次/min,血氧饱和度99%(呼吸机支持)。WBC 26.90×109/L,N% 94.60%,CRP 145.6 mg/L,PCT >100.00 ng/ml,肌酐171.0 μmol/L,尿素 8.84 mmol/L,白介素-6 2850.00 pg/ml。
入院诊断:①脓毒性休克;②急性化脓性阑尾炎伴弥漫性腹膜炎;③唐氏综合征。
-
患者入院急行开腹探查术,术后转重症监护病房(ICU),呼吸机辅助通气、腹腔闭式引流改善腹腔顺应性、右侧颈内放置中心静脉导管(CVC),同时,液体复苏、血管活性药物维持血压并经验性抗感染治疗。入院第5 d,微生物学检查:多重耐药鲍曼不动杆菌(MDRAB)及星座链球菌感染。遂改用头孢曲松+舒巴坦,治疗6 d后,患者腹腔感染好转,血流动力学稳定,拔除气管插管。
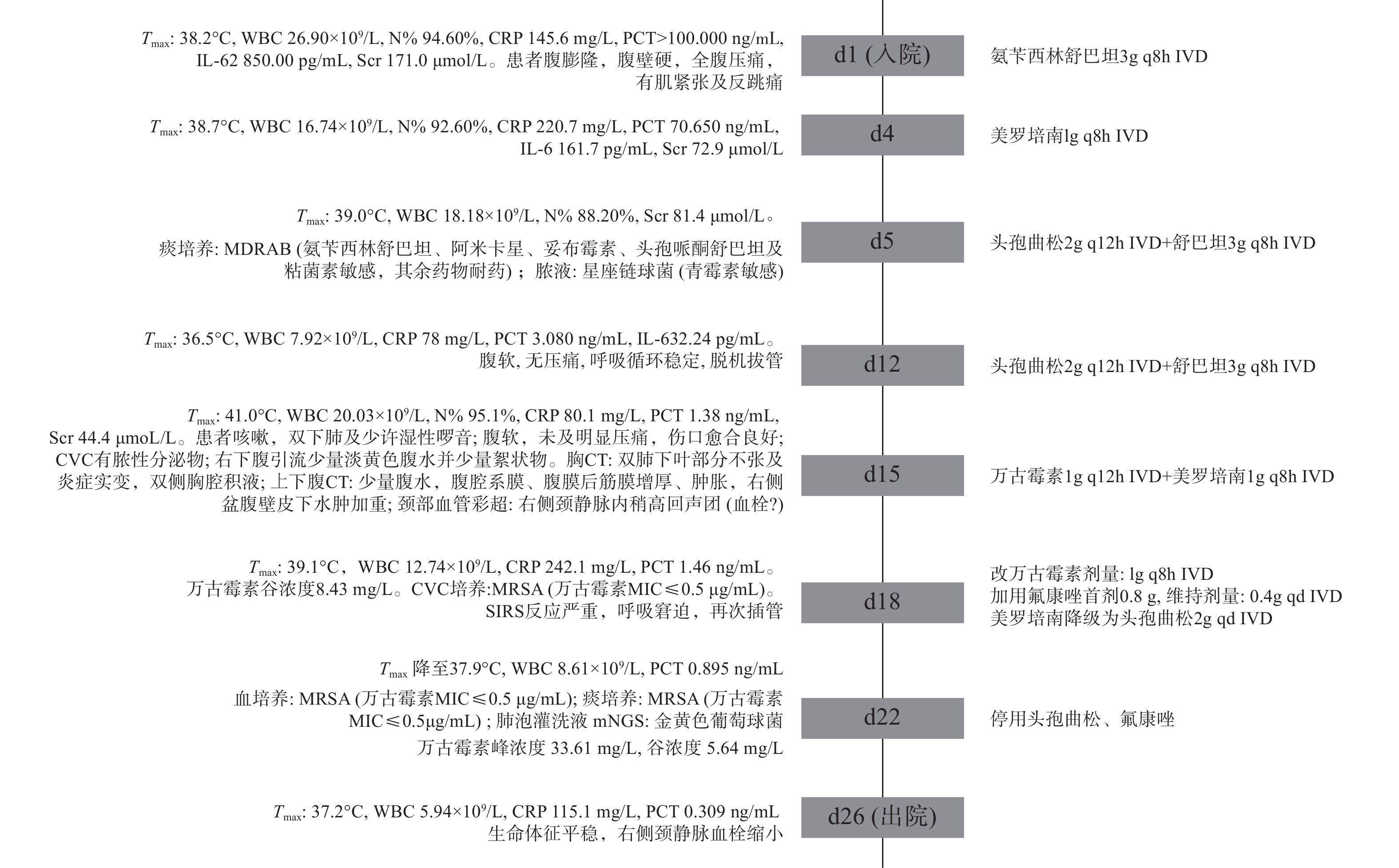
入院第15 d,患者再次高热,留置导管处出现脓性分泌物且颈部血管彩超提示附壁血栓形成,胸CT提示双肺炎症。立即拔除CVC送血培养,当天CVC细菌涂片回报:少量革兰阳性球菌,升级抗感染方案,入院第18~21 d,分别从CVC、血培养、痰培养分离出耐甲氧西林金黄色葡萄球菌(MRSA),肺泡灌洗液宏基因组测序(mNGS):金黄色葡萄球菌。确诊MRSA导致复杂导管相关性血流感染,并继发肺部感染。根据患者症状体征、药敏试验结果及血药浓度监测结果等,调整抗感染治疗方案,同时辅以那曲肝素钙(0.4ml q12h ih)抗凝治疗。第26 d病情好转,患者及家属要求出院。住ICU期间重要临床信息及抗感染治疗经过见图1。
-
患者入院立即行腹腔引流及抗感染治疗,并于抗感染治疗之前,留送标本,但初始抗感染选用了氨苄西林舒巴坦。临床药师认为,社区获得性腹腔感染常见病原菌主要为肠道菌群,其标准抗菌治疗应包括抗肠杆菌、需氧链球菌、专性厌氧菌感染的药物[4]。目前全球革兰阴性肠杆菌科对氨苄西林舒巴坦的耐药性很强,从腹腔感染中最常分离出的10种细菌对氨苄西林舒巴坦均不敏感[5]。基于上述证据,且患者为重症感染,临床药师建议经验性抗感染药物更换为哌拉西拉他唑巴坦(4.5g q8h)或美罗培南(1g q8h),医师采纳。
-
患者入院第15 d,再次高热、脓毒症再袭,感染来源首先考虑导管,其次肺部,另外原发病灶也未完全控制,故调整抗感染方案为:万古霉素联合美罗培南。2 d后患者仍高热、气促、呼吸窘迫,临床药师分析抗感染疗效不佳的可能原因,并给出相应建议:①抗菌药物剂量不足,万古霉素个体化差异较大,建议监测万古霉素血药浓度以便及时调整[6]。②治疗方案未覆盖致病菌,根据念珠菌评分(CS),该患者目前4分(脓毒症2分、腹部手术1分、肠外营养1分),念珠菌感染风险较高,建议启动抗真菌抢先治疗。③患者微生物培养结果为革兰阳性菌且PCT< 2ng/ml, 耐药革兰阴性菌感染可能较小,美罗培南降阶梯为头孢曲松,避免长期使用广谱抗菌药导致二重感染。医师采纳临床药师建议。
入院第18~21 d,导管、血、痰培养均为MRSA,提示肺部感染继发于STP,以往研究也证明继发于STP的脓毒性栓子更常见于肺部[7],治疗应以血流感染为主同时兼顾肺部。在病原菌明确的情况下,药师建议停用氟康唑及头孢曲松。万古霉素在肺泡上皮衬液(ELF)中浓度/血药浓度为5%~50%,肺内分布良好,表明在治疗STP同时能在肺部达到有效治疗浓度,疗程需要延长至4~6周[8]
-
⑴万古霉素初始给药方案制订:患者初始给予万古霉素1g q12h,连续使用3 d疗效不佳。临床药师评估治疗方案后,发现未结合万古霉素的药动学/药效学(PK/PD)特点及重症患者的病、生理情况来设计给药,导致万古霉素未达到PK/PD目标靶值。根据《2020万古霉素治疗严重MRSA感染的治疗药物监测》共识指南[6],≥12岁儿科患者初始治疗剂量为60~70 mg/(kg·d),不超过3.6g 为宜,患者体重65 kg,初始给药剂量3~3.6 g/d较合适。指南同时推荐MRSA引起重症感染的成人患者给予负荷剂量以助于快速达到目标稳态浓度,控制感染,而儿科患者缺乏大型前瞻性研究,但回顾性研究提示接受万古霉素负荷剂量(20~25 mg/kg)的儿童与未接受的相比,可能更快达到初始目标谷浓度,且不增加肾毒性[9]。该患者近期高热、心率偏快,处于高代谢状态,且处于肾功能亢进状态(肌酐清除率220 ml/min),可能进一步加快万古霉素代谢,故临床药师认为该患者初始给药方案:首剂1.5g+维持1g q8h,更利于快速达标、控制感染,同时进行治疗药物监测,便于后续剂量调整。
⑵万古霉素剂量优化:第4 d万古霉素血药浓度监测结果为Cmin 8.43 mg/L,根据《中国万古霉素治疗药物监测指南》[10],对于严重MRSA感染的患者,建议万古霉素目标谷浓度维持在10~20 mg/L。因此,临床药师建议增加一个给药间隔,以提高药物血药浓度,并持续监测。治疗第6 d,万古霉素血药浓度:Cmax 33.61 mg/L,Cmin 5.64 mg/L,谷值依然未达标,但患者体温下降,症状及感染指标均好转,医生考虑抗感染治疗有效,询问临床药师是否需要调整万古霉素给药方案。临床药师经查阅最新共识指南[6],建议通过监测药物浓度-时间曲线下面积(AUC)来指导万古霉素的剂量调整,推荐个体化给药AUC/MIC目标值为400~600以达到最佳的临床疗效。同时文献[11]指出谷浓度可能不是AUC最佳替代,在几种不同剂量方案下AUC范围很宽,但可产生相似谷值;同样相似AUC,谷值也不尽相同。因此,临床药师根据所测峰谷浓度,依据线性梯形法则计算万古霉素AUC0-24为415 mg·h/L,故建议维持原剂量治疗。经密切监测患者肾功能并观察各项感染指标、体温情况,均持续好转,提示治疗有效且未发生肾功能损伤等不良反应。为此,临床药师建议万古霉素根据AUC调整更精确,相比单点暴露的谷浓度,AUC为累积药物暴露总量,以往是将谷浓度转化为每日最小AUC,存在一定局限性,尤其在重症患者中,药物代谢受多方面因素影响,谷浓度可能不足以指导所有患者的剂量调整,而AUC0-24h则代表该时间段的平均浓度,可更好体现目标实现率与疗效的关系,指导剂量优化。
-
导管相关性血流感染和血栓形成互为因果,导管周围出现血栓,亦增加了微生物定植和菌血症的风险[12]。关于化脓性血栓静脉炎是否给予全身抗凝治疗尚存在争议,由于STP很少见,缺少临床试验,无法研究可能的疗效和安全性结果或获益可能超过风险的亚群[13]。Uptodate[14]建议,STP采取抗凝治疗情况包括:在适宜抗生素治疗下血栓仍扩散;脓毒症在48~72 h的适宜抗菌药物治疗后仍不受控制;高凝状态。《2018美国血液病学会儿童静脉血栓栓塞症管理指南》指出抗凝或不抗凝都是合理的[15]。临床药师经查阅文献,提示颈静脉、门静脉血栓一般推荐在血栓扩大或经抗生素治疗后进展才抗凝治疗[13]。有学者[16]对28名STP住院儿科患者的抗凝治疗时间及安全性进行了为期10年的回顾性研究,其中25名患者接受抗凝治疗,疗程约12周,血栓清除率48%,尽管治疗结束时血栓溶解率较低,但感染复发风险低,没有发现延长抗凝的优势,同时抗凝安全性良好。
临床药师综合现有证据,建议仅在血栓扩展或复发的情况下考虑抗凝,疗程12周;抗凝的安全结局除出血,还应考虑到血栓破裂引起感染灶扩散及脓肿出血性转化。结合本例患者情况,STP诊断明确,肺部感染继发于STP,微生物培养得到证实,抗感染方案已优化,为进一步防止血栓扩散,可考虑抗凝。同时复查D-二聚体、血栓弹力图,评估患者出血与血栓风险,发现患者D-二聚体从入院开始持续升高至15.45mg/L,同时凝血因子活性升高,表明其血栓形成风险高,出血风险低。故临床药师建议抗感染同时给予那曲肝素钙0.4ml q12h。经过抗凝及抗感染治疗,患者右侧颈静脉附壁血栓缩小,未出现肺栓塞及感染性心内膜炎。
-
本病例患者初始因腹内脓毒症入院,经过积极引流、抗感染治疗后腹腔感染好转,但后期继发院内感染,导致脓毒症再袭。提示重症患者病情多变,临床药师需要时刻关注患者症状、体征的改变,并根据感染部位、严重程度及时调整抗感染方向。同时,重症感染患者治疗成功的关键在于确保抗菌药物给药剂量能达到PK/PD目标靶值,合理进行个体化血药浓度监测是调整并优化重症患者给药方案的基础,临床药师借助TDM,对于监测数据的准确解读及应用,实现了重症儿科患者的精准化治疗。化脓性血栓静脉炎治疗方案制订过程检索了国内外指南及文献,充分考虑了抗凝治疗的时机及必要性,保障了患者用药安全及疗效。
Analysis of drug therapy in a patient with pulmonary infection secondary to suppurative thrombophlebitis
-
摘要:
目的 探讨在治疗化脓性血栓静脉炎继发转移性肺部感染患者过程中药学监护的作用。 方法 回顾性分析1例确诊为化脓性血栓静脉炎,并继发肺部转移性感染患者的治疗及临床药师参与监护的全过程,评价抗菌药物的使用,并探索化脓性血栓性静脉炎治疗中抗凝管理的经验。 结果 临床药师基于感染部位、脓毒性血栓特点、万古霉素血药浓度监测、抗菌药物代谢动力学/药效学特性等,在抗感染方案调整、万古霉素个体化治疗优化、抗凝时机等方面为临床医师及患者提供全面药学服务,患者全身感染及脓毒性血栓得到有效控制,促进了化脓性血栓静脉炎患者的治疗。 结论 临床药师能在重症患者治疗团队中发挥重要作用,提高抗菌药物的合理使用。 Abstract:Objective To explore the role of pharmaceutical care in the treatment of patients with pulmonary infection secondary to suppurative thrombophlebitis. Methods The treatment of a patient diagnosed with pulmonary metastatic infection secondary to suppurative thrombophlebitis and the whole process of clinical pharmacists participating in the monitoring were analyzed retrospectively. The use of antibiotics was evaluated, and the experience of coagulation management in suppurative thrombophlebitis was explored. Results Based on the infection site, characteristics of septic thrombus, monitoring of vancomycin blood concentration, pharmacokinetics and pharmacodynamics characteristics of antibiotics, clinical pharmacists provided comprehensive pharmaceutical services for clinicians and patients in terms of anti-infection scheme adjustment, optimization of vancomycin individualized treatment, anticoagulant timing. Patient’s systemic infection and septic thrombus can be effectively controlled and which promotes the treatment of patients with suppurative thrombophlebitis. Conclusion Clinical pharmacists can play an important role in the treatment team of severe patients to improve the rational use of antibiotics. -
心脑血管疾病是心脏血管和脑血管疾病的统称,泛指由于高脂血症、血液黏稠、动脉粥样硬化、高血压等所导致的心脏、大脑及全身组织发生的缺血性或出血性疾病。心脑血管疾病是一种严重威胁人类健康的常见病,具有高患病率、高致残率和高死亡率的特点。这种疾病也对我国人民的健康和医疗卫生事业的发展带来了巨大的挑战。而在心脑血管疾病中,又以缺血性心脏病和缺血性脑卒中最为常见[1-3]。
黄酮类化合物(flavonoids)是一类广泛存在于自然界植物中的次生代谢产物。是一种以黄酮(2-苯基色原酮)为母核而衍生的一类黄色色素,其中包括黄酮的同分异构体及其氢化和还原产物[4]。它在植物的生长、发育、开花、结果以及抗菌防病等方面起着重要的作用。本文将对目前黄酮类化合物抗心脑血管疾病的作用研究进展作一综述。
1. 黄酮类化合物对缺血性心脏病的保护作用
早在1938年,Szent-Gyorgyi等研究发现来自于柠檬的黄酮类化合物橘皮苷具有强化毛细血管的作用,该项功能将有助于改善心脏微循环的水平,从而产生保护作用[5]。此后,一项名为Zutphen Elderly Study的流行病学研究探讨了膳食类黄酮摄取量与冠心病风险之间的相关性。该研究对65岁至84岁的老年男性黄酮类摄取量进行了统计,结果显示膳食类黄酮摄取量与冠心病引起的死亡之间呈明显负相关,同时与心梗发病率之间也呈弱负相关 [6]。在欧洲,荷兰科学家对黄酮醇类和黄酮类摄入量与冠心病死亡率和中风发生率之间做了分析,结果显示摄入量大于30 mg/d者两种疾病的发病风险仅为摄入量最低者的三分之一,且该项调查已排除了高胆固醇、高血压、饮酒、吸烟等心脑血管疾病常见危险因素的影响。而另一项针对饮茶人群的研究表明茶叶中富含的茶叶类黄酮可以很好地预防缺血性心脏病的发生 [7]。这些研究均提示我们黄酮类物质可能发挥较强的抗氧化作用,从而降低冠心病的发病率和死亡率。
2. 黄酮类化合物对缺血性脑卒中的保护作用
与心肌缺血类似,缺血性脑卒中同样严重威胁人类的生命健康。而与心肌缺血不同的是,损伤部位是人类神经行为的中枢—脑组织,因此,临床表现更为复杂。黄酮类化合物作为一种常见且重要的中药成分被较多的实验证明其具有抗缺血性脑卒中的作用。
研究表明从中药灯盏细辛中提取出来的黄酮类活性成分灯盏花素可以起到抗脑缺血的作用,其作用主要通过改善血液流变学、缩小脑组织梗死面积以及减少脑海马区域细胞凋亡数来实现[8-9]。此外,本课题组从传统中药中提取出来的黄酮类活性成分菸花苷,在实验中被证明同样具有确切的保护脑缺血损伤的作用。实验中急性脑缺血的大鼠在注射菸花苷后其生存率较对照组有大幅提升,同时缺血梗死面积显著缩小[10-11],在各个时间点对给药组和对照组进行神经行为学评价如mNSS评分、提尾实验等,发现注射菸花苷的大鼠其行为学得分逐渐降低,提示神经功能逐渐趋向好转。此外,该实验还对各组大鼠脑电图和脑组织含水量进行了测定,结果表明,给予菸花苷治疗的大鼠脑电图消失的时间显著延长,同时其脑组织含水量显著降低,改善了脑水肿情况 [12]。证实了菸花苷对动物的实验性脑梗塞及缺血后再灌注引起的组织损伤有明显的预防和治疗作用。
3. 黄酮类化合物对缺血性心脏病及缺血性脑卒中的保护作用的机制研究
研究发现,缺血性心脏病和缺血性脑卒中的病理机制类似,可以归纳为氧化性损伤、钙超载、炎症反应、细胞凋亡及血小板凝集、自噬等。这几种因素之间相互作用,相互影响,形成多个复杂的调控网络,从而造成一系列病理级联反应。而黄酮类化合物可以通过对上述各因素的抑制作用来保护损伤的心肌组织和脑组织。
3.1 抗氧化
现代医学研究表明,在心肌缺血发生时,人体内会产生较多的氧自由基,同时机体清除氧自由基的能力下降,使得堆积的氧自由基在心肌细胞中发生过氧化反应,从而破坏心肌细胞的结构和功能,导致心肌缺血进一步加重[13]。研究发现,超氧化物酶(SOD)作为生物体内清除自由基的首要物质,可减弱氧自由基对细胞造成的损伤,同时还具有修复受损细胞的功能,其活性高低可反映机体清除自由基能力的大小[14];丙二醛(MDA)则作为脂质过氧化物反应的产物,常被用于评价机体氧化应激损伤的严重程度[15];一氧化氮(NO)是我们熟知的生物体内反应极强的自由基,在机体发生心肌缺血时,该物质在血清中的水平明显下降。实验表明,葡萄籽中富含的原花色素可以有效地清除自由基,从而稳定心肌细胞膜,对心肌产生保护作用[16-17]。另一项研究以异丙肾上腺素作为诱导的急性心肌缺血大鼠为模型,探索了布渣叶总黄酮对心肌缺血的作用,结果显示,布渣叶总黄酮可明显降低大鼠血清中乳酸脱氢酶(LDH)、肌酸激酶(CK)以及心肌组织中MDA的含量,同时心肌组织中SOD和NO的活性也得到提高[18]。揭示了黄酮类化合物通过抗氧化作用来产生保护心肌组织的作用。
近年来,氧化应激学说同样也在脑缺血性疾病中被广泛研究。该机制不仅可以直接造成细胞破坏,使脑细胞坏死,还可以通过介导线粒体途径,神经细胞膜结构以及DNA修复酶和转录因子等间接地导致脑细胞凋亡。研究发现,注射天然黄酮类化合物木犀草素的脑缺血大鼠SOD、过氧化氢酶(CAT)活性相较于对照组明显提升,而MDA的含量则显著降低,该结果提示我们木犀草素可以加强机体清除氧自由基的能力,从而产生脑保护作用[19]。而在另一项体外研究中,中药黄芩中的黄酮类化合物黄芩苷可以抑制外源性和内源性过氧亚硝基阴离子诱导的神经毒性作用,保护人源神经母细胞瘤细胞(SH-SY5Y)神经细胞系[20]。同时,从传统中药红花中提取出来的黄酮类成分菸花苷,也在此前的实验中被证实可以显著降低脑组织中MDA的含量,提高SOD活性[12]。以上结果表明,黄酮类化合物发挥抗心肌缺血及脑缺血的作用与提高机体抗氧化应激的能力有密切的关系。
3.2 抑制炎症反应
炎症反应广泛地存在于各种疾病的病理机制中,其主要通过致炎因子和炎性介质来介导一系列的链式反应。当炎症反应发生在缺血的心肌细胞时,会进一步加剧细胞的缺血和缺氧 [21]。在炎症反应中,具有代表性的重要炎症因子有白介素家族,如IL-1β、IL-6以及肿瘤坏死因子(TNF-α)等,这些炎症因子多出现在炎症反应通路的下游,直接影响并加剧炎症反应的发生和发展。而另一种重要的转录因子Kappa-B(NF-κB),作为一种氧化还原敏感因子在炎症反应中同样扮演了重要的角色,其介导的一系列炎症因子如上述的白介素家族、趋化因子、炎性小体等在心肌细胞缺血损伤中起到重要的作用[22-24]。以往的研究表明,香青兰总黄酮可以抑制心肌缺血大鼠心肌组织中的炎症因子白介素IL-1、IL-6和TNF-α的水平,使炎症因子减少释放,从而降低心肌组织中中性粒细胞的浸润,以达到保护心肌的作用[25]。另一项研究也发现,银杏黄酮同样可以抑制心肌组织中中性粒细胞的浸润,其作用主要通过下调NF-κB和细胞间黏附因子-1(ICAM-1)的表达来实现[26]。
与此类似,在机体发生缺血性脑卒中的时候,各类炎症因子依然扮演了重要的角色。研究发现,灯盏细辛在治疗脑梗死时可以显著降低TNF-α、IL-6的含量,从而减轻炎症反应[27]。在另一项对黄酮类化合物山奈酚的研究中发现,其抗炎作用已在细胞层面得到了证实。它可降低促炎因子的产生和mRNA表达,如胸腺基质淋巴细胞生成素(TSLP)、IL-8等[28],此外,在以PC12细胞作为研究对象的体外实验中,人们发现加入山奈酚处理后,该组细胞的炎性相关蛋白环氧化酶(COX2),诱导型一氧化氮合酶(iNOS)以及核因子NF-κB水平明显下调,且细胞活力随着的山奈酚的浓度增加而逐步增长;进一步的检测发现,对照组的磷酸化P38丝裂原活化蛋白激酶(P38-MAPK)表达升高,而山奈酚组表达降低,而当加入P38-MAPK抑制剂后发现对照组的炎性相关蛋白水平降低[29],该结果提示我们黄酮类化合物山奈酚可以通过抑制P38-MAPK信号通路来对抗机体病理性炎症反应[30],进而产生脑细胞保护作用。由此可见,黄酮类化合物主要通过影响炎症因子的表达和释放来发挥抗炎的作用。
3.3 抑制细胞凋亡
细胞凋亡又称为程序性细胞死亡,是机体为了维持内环境稳定,通过基因控制的细胞自主而有序的死亡,涉及了一系列的基因激活、表达以及调控作用,与各种信号通路、免疫应答以及上述提到的炎症反应有着密不可分的联系。细胞凋亡是心肌缺血再灌注损伤的重要病理机制之一。目前与细胞凋亡相关的基因有Bcl-2家族,Caspase家族等,相关通路有NF-κB信号通路、丝裂原活化蛋白激酶MAPK信号通路、磷脂酰肌醇-3激酶/蛋白激酶B(PI3K/AKT)信号通路等。这些基因同时参与了细胞凋亡的诱发和抑制。在一项研究中发现,我国瑶族传统草药成分铜钻总黄酮可以明显降低已形成心肌缺血再灌注损伤的大鼠心肌组织中Bax蛋白的表达,该蛋白可以促进细胞凋亡,同时实验还发现铜钻总黄酮还可以升高抗凋亡的Bcl-2蛋白的表达,从而抑制细胞凋亡,避免心肌缺血再灌注损伤的进一步加重[31]。在另一项研究中,科研人员发现来源于印度崖豆的黄酮类化合物不仅可以降低Bax蛋白的表达,升高Bcl-2蛋白的表达,还可以提升心肌组织中结构氮氧化合成酶(cNOS)的活性,同时抑制诱生型一氧化氮合酶(iNOS)活性,从而显著改善心肌缺血再灌注大鼠的心肌组织病理学形态,其实验组的心肌细胞形态、结构和排列较之对照组更为完整和规律[32]。同时在MAPK信号通路中c-Jun氨基末端激酶(JNK)和P38蛋白激酶可促进细胞的凋亡。研究发现玫瑰中黄酮类化合物可显著下调大鼠心肌组织中磷酸化JNK和P38的表达,从而抑制心肌细胞的凋亡 [33]。而另一条重要的信号转导通路PI3K/AKT在细胞的增殖、凋亡、代谢中也发挥了重要的生物学作用,其可抑制细胞凋亡的进程[34]。其中活化的AKT进入细胞质与细胞核后,可以调节Caspase家族中Caspase-3的表达,同时还可以调节内皮型一氧化氮(eNOS)以及抗凋亡因子Bcl-2和促凋亡因子Bax的表达[35-36]。实验发现,玉郎伞查尔酮可以激活PI3K/AKT信号通路,抑制大鼠心肌细胞的凋亡,从而产生抗心肌缺血的作用[37]。此外,有研究表明黄芩茎叶总黄酮可以降低发生心肌缺血再灌注损伤的大鼠心肌细胞的凋亡率,其作用可能与降低Caspase-3基因mRNA和蛋白表达有关[38-39]。
细胞凋亡同时也是缺血性脑卒中发生发展的一个重要病理机制。临床研究发现,认知障碍是缺血性脑卒中发病后的一项重要并发症,它严重影响患者的预后和生活质量。因此,大脑中负责学习记忆和认知的海马区成为了科学家们重点关注的对象。其中CA1区的神经元对脑缺血缺氧较为敏感,容易受到损伤,而CA3区及DG区的神经元则相对耐受[40]。尼氏体是神经元胞体和树突内的嗜碱性颗粒或小斑块,由游离的核糖体和粗面内质网构成,对缺血变化非常敏锐[41]。课题组在对黄酮类化合物菸花苷的一项研究中发现,缺血再灌注的大鼠海马区神经元大小不一,胞质不规则淡染,胞核皱缩变形,部分细胞脱失明显,CA1区锥体细胞和 DG区的颗粒细胞排列松散,CA3区锥体细胞排列散乱,表明大鼠发生急性脑缺血再灌注损伤后神经细胞受损严重,与之相比,使用菸花苷处理的MCAO大鼠神经元虽也出现了细胞淡染,大小不均,部分胞体肿胀,CA1区及DG区排列稍显混乱,但整体的形态接近正常,病理损伤明显减轻。同时,在尼氏体方面,模型组整体淡染,皮层的尼氏体大大减少,海马区尼氏体极少,表明造模后神经元功能受到损伤。与模型组相比,菸花苷组皮层尼氏体数目更多,个体更大,染色较均匀,海马区尼氏体虽多为颗粒状,个体稍小,但数目明显增多,说明神经元蛋白合成有所增加,较为活跃[42]。因此,我们可以得出结论,菸花苷通过促进神经元蛋白的合成,抑制神经细胞的凋亡,保持神经元的活性来提高机体抗脑缺血的功能。同样,黄芩苷在用于脑缺血动物模型时,也可以明显改善实验动物的认识记忆能力[43],还通过下调促凋亡基因Bax的表达,下调Bax/Bcl-2的比值,降低COX-2的表达来抑制神经细胞凋亡[44]。以上研究表明,黄酮类化合物通过抑制细胞凋亡来进一步保护心脑组织免受缺血再灌注的损伤。
3.4 抑制钙超载
研究发现,当心肌发生缺血时,心肌细胞线粒体中Na+/K+-ATP酶和Ca2+-ATP酶活性下降,使线粒体对钙离子的摄入减少,同时包浆内的钠离子含量升高,造成Na+ -Ca2+交换增加,从而发生钙超载 ,加重心肌缺血的临床症状[45]。研究发现,玉郎伞黄酮能够提高心肌组织中的Na+/K+-ATP酶和Ca2+-ATP酶活性,减轻细胞内钙离子超载的程度,改善缺血再灌注造成的心肌损伤[46];从传统中药香青兰中提取的香青兰总黄酮也可以提高心肌组织中的ATP酶含量,保持线粒体的活性和结构完整性,使其功能得到发挥,从而抑制钙超载的发生[47]。
3.5 抗血小板聚集
在正常的生理状态下,血栓素花生四烯酸(TXA2)与环前列腺素(PGI2)处于一种相对平衡的状态。而在心肌受到缺血再灌注损伤后,该平衡即被打破。此时,心肌内皮细胞受损,导致PGI2合成减少而TXA2作用增强,进一步引起血小板大量聚集,从而加重心肌缺血的程度。研究表明,黄酮类化合物可以发挥抗血小板聚集的作用。如从黄顶茜草中分离出的硫酸黄酮能够阻断TXA2受体而发挥抗血小板凝集的作用 [48]。同样的,白桂芦苇中的黄酮类化合物也可以抑制血小板的聚集,从而起到保护心肌的作用[49]。上述现象的发生机制可能与黄酮类化合物抑制环氧合酶,提高血小板环磷酸腺苷(cAMP)合成,阻断TXA2受体,提高PGI2水平有着直接的联系。
3.6 自噬通路
自噬是近几年科学界的一个研究热点,其因开启细胞循环自身物质的新纪元而备受全世界的关注 [50-52]。自噬根据发生过程分为三类:巨自噬,微自噬,分子伴侣介导的自噬。目前研究一般集中于巨自噬,其一般过程为:自噬前体的形成,自噬前体延长包裹底物形成自噬小体,自噬小体与溶酶体融合形成自噬溶酶体最终降解[53-55]。在脑卒中的发生过程中,自噬起到了关键的保护作用。课题组在MCAO大鼠模型中发现菸花苷可以增加大鼠脑缺血再灌注后缺血半暗带的自噬小体数目,增强LC3的表达,提高活性形式 LC3-II 在LC3表达中所占的比例,增强参与吞噬泡形成的重要相关蛋白 BECN1 蛋白的表达,降低参与自噬溶酶体降解的重要蛋白 SQSTM1 蛋白的表达,降低自噬相关通路雷帕霉素靶蛋白依赖性途径中关键蛋白 phospho-mTOR 的表达,上调 BECN1、Atg7 mRNA 的表达,下调SQSTM1mRNA的表达。由此可知,菸花苷对大鼠脑缺血再灌注后缺血半暗带的自噬水平有促进作用。同时在体外,在人源神经母细胞瘤细胞(SH-SY5Y)细胞株上建立模拟体内缺血再灌注的缺复氧模型,结果显示,菸花苷同样可以增加SH-SY5Y细胞内自噬小体的生成,增加LC3的表达,提高自噬体膜标志性蛋白LC3-II表达含量,增强BECN1蛋白的表达,降低SQSTM1蛋白的表达,增强促进细胞内自噬流的进程[42, 56]。由此可知,黄酮类化合物菸花苷可通过自噬来发挥神经保护作用。
4. 小结和展望
黄酮类化合物作为一种常见的天然化合物,存在于自然界的许多植物以及传统中药中。随着科学技术的进步,人们发现这类化合物具有诸多的生物活性,而其强大的药理作用也屡见报道。如降低血管的脆性,改善血管的通透性、降低血脂和胆固醇,防治老年高血压、脑溢血、冠心病、心绞痛、扩张冠状血管,增加冠脉流量等。在这些药理作用中,其抗心脑缺血的作用对于临床上治疗和预防相关疾病显得尤为重要。在上文中,我们列举了许多不同种类的黄酮类化合物在心脑血管疾病中的作用,这些活性成分有的可以直接通过改善血管通透性、缩小梗死组织面积来保护心脑血管组织,有的则通过分子信号通路来产生保护作用。随着研究的推进,它们的作用机制也进一步地得到阐释。可以肯定的是,黄酮类化合物能够为人类治疗和预防心脑血管疾病提供新的治疗思路。当然目前很多实验仅涉及到分子机制中的某个环节,而对于完整的调控过程,精准的作用靶点还有待研究发现。只有通过这一系列系统科学的研究,才能够更好地为心脑血管疾病的治疗提供理论依据,从而进一步在临床得到广泛的应用。
-
[1] LIPE D N, FORIS L A, KING K C. Septic Thrombophlebitis [M]. StatPearls. Treasure Island (FL); StatPearls Publishing, 2021. [2] MERMEL L A, ALLON M, BOUZA E, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Disea-ses Society of America[J]. Clin Infect Dis,2009,49(1):1-45. doi: 10.1086/599376 [3] FALAGAS M E, VARDAKAS K Z, ATHANASIOU S. Intravenous heparin in combination with antibiotics for the treatment of deep vein septic thrombophlebitis: a systematic review[J]. Eur J Pharmacol,2007,557(2-3):93-98. doi: 10.1016/j.ejphar.2006.11.068 [4] 吴秀文, 任建安. 中国腹腔感染诊治指南(2019版)[J]. 中国实用外科杂志, 2020, 40(1):1-16. [5] HACKEL M A, BADAL R E, BOUCHILLON S K, et al. Resistance rates of intra-abdominal isolates from intensive care units and non-intensive care units in the United States: the study for monitoring antimicrobial resistance trends 2010-2012[J]. Surg Infect (Larchmt),2015,16(3):298-304. doi: 10.1089/sur.2014.060 [6] RYBAK M J, LE J, LODISE T P, et al. Therapeutic monitoring of vancomycin for serious methicillin-resistant Staphylococcus aureus infections: a revised consensus guideline and review by the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, the Pediatric Infectious Diseases Society, and the Society of Infectious Diseases Pharmacists[J]. Am J Health Syst Pharm,2020,77(11):835-864. doi: 10.1093/ajhp/zxaa036 [7] YE R, ZHAO L, WANG C H, et al. Clinical characteristics of septic pulmonary embolism in adults: a systematic review[J]. Respir Med,2014,108(1):1-8. doi: 10.1016/j.rmed.2013.10.012 [8] CHAVES F, GARNACHO-MONTERO J, DEL POZO J L, et al. Diagnosis and treatment of catheter-related bloodstream infection: clinical guidelines of the Spanish society of infectious diseases and clinical microbiology and (seimc) and the Spanish society of Spanish society of intensive and critical care medicine and coronary units (semicyuc)[J]. Med Intensiva (Engl Ed),2018,42(1):5-36. doi: 10.1016/j.medin.2017.09.012 [9] DOLAN E, HELLINGA R, LONDON M, et al. Effect of vancomycin loading doses on the attainment of target trough concentrations in hospitalized children[J]. J Pediatr Pharmacol Ther,2020,25(5):423-430. [10] YE Z K, CHEN Y L, CHEN K, et al. Therapeutic drug monitoring of vancomycin: a guideline of the Division of Therapeutic Drug Monitoring, Chinese Pharmacological Society[J]. J Antimicrob Chemother,2016,71(11):3020-3025. doi: 10.1093/jac/dkw254 [11] PATEL N, PAI M P, RODVOLD K A, et al. Vancomycin: we can’t get there from here[J]. Clin Infect Dis,2011,52(8):969-974. doi: 10.1093/cid/cir078 [12] VAN ROODEN C J, SCHIPPERS E F, BARGE R M, et al. Infectious complications of central venous catheters increase the risk of catheter-related thrombosis in hematology patients: a prospective study[J]. J Clin Oncol,2005,23(12):2655-2660. doi: 10.1200/JCO.2005.05.002 [13] VALERIO L, RIVA N. Head, neck, and abdominopelvic septic thrombophlebitis: current evidence and challenges in diagnosis and treatment[J]. Hamostaseologie,2020,40(3):301-310. doi: 10.1055/a-1177-5127 [14] DENIS S, MBBS, FRACP, et al. Catheter-related septic thrombophlebitis[EB/OL]. UpToDate, 2020, 12, 08https://www.uptodate. com/contents/catheter-related-septic-thrombophlebitis. [15] MONAGLE P, CUELLO C A, AUGUSTINE C, et al. American Society of Hematology 2018 Guidelines for management of venous thromboembolism: treatment of pediatric venous thromboembolism[J]. Blood Adv,2018,2(22):3292-3316. doi: 10.1182/bloodadvances.2018024786 [16] KOO J, PONG A, DORY C, et al. Management and outcomes of pediatric septic thrombophlebitis: a case series[J]. Pediatr Hematol Oncol,2020,37(4):344-352. doi: 10.1080/08880018.2020.1733147 期刊类型引用(16)
1. 林启炫,杜灿凯,林稚凯,赵秀娟,刘姚. 黄酮类化合物的生物活性及应用研究. 现代食品. 2024(02): 92-97 .  百度学术
百度学术2. 刘莉,王凤荣. 基于网络药理学和分子对接法研究参七解郁方治疗双心疾病的分子机制. 安徽医药. 2024(05): 909-914+1065 .  百度学术
百度学术3. 钟智,徐维那,郭帅,路镜达,邱景良,王记成. 复合益生菌后生元的功效及有益代谢产物的研究. 食品工业科技. 2024(12): 160-168 .  百度学术
百度学术4. 赵敏霖,张萌,张浩,张丽娟,姜丰,余四娜,王莉兴,李清. 黄酮类化合物的作用及在牛生产中的应用研究进展. 饲料研究. 2024(09): 132-137 .  百度学术
百度学术5. 宋鹏鹏,郭燕可,关东升,马鸣,崔应麟. 基于网络药理学、分子对接及实验验证探讨益气通脉散抗脑缺血再灌注损伤的作用机制. 中药新药与临床药理. 2024(07): 1016-1027 .  百度学术
百度学术6. 余柠未,丁燕,李卫忠,李云涛,刘振环. 高效液相色谱法测定桃胶中3种主要类黄酮物质含量. 江苏农业科学. 2024(15): 203-207 .  百度学术
百度学术7. 冉雯仪,吴艳萍,黄毅娜,高鸿. 黄酮类小分子与细胞膜的相互作用. 食品工业. 2024(12): 89-94 .  百度学术
百度学术8. 周茂琳,王怿,李雪菲,杨灿,马梦娇,阮铭,王杰,徐浩,施杞,王佑华,梁倩倩. 基于网络药理学探讨脏痹方治疗TNF-Tg小鼠类风湿关节炎并发心肌肥厚的疗效研究. 世界科学技术-中医药现代化. 2024(11): 2937-2950 .  百度学术
百度学术9. 张瑶,葛飞,申冰清,罗亚敏,侯鉴宸,潘菽弢,王春国,邱月华,陶晓华. 基于UHPLC-Q-Exactive Orbitrap MS的桃核承气汤化学成分快速鉴定. 中南药学. 2023(01): 28-36 .  百度学术
百度学术10. 寇宇,管婷婷,何鑫,刘大军,宋永,孙庆申. 生长期及发酵处理对东北油豆角黄酮含量的影响. 食品安全质量检测学报. 2023(06): 302-309 .  百度学术
百度学术11. 江春阳,邓乔晟,王丹,许凌峰,杨青山,张华,杨勤,石汝杰,周浓. 响应面-Box-Behnken设计优化地参中总黄酮含量检测方法以及不确定度评定. 食品与发酵工业. 2023(14): 280-287 .  百度学术
百度学术12. 陈心雨,李琳,刘宏飞,刘念,王超凯,张磊,李觅,常少健,蔡海燕,彭奎,郭杰. 桂圆果核黄酮提取工艺及抗氧化活性研究. 食品与发酵科技. 2023(04): 44-50 .  百度学术
百度学术13. 张文静,徐浩群,李冲,韩冰冰,侯冠群,张义敏. 基于阴阳学说探讨自噬与缺血性脑卒中相关性. 辽宁中医药大学学报. 2023(10): 147-153 .  百度学术
百度学术14. 寸睿,陈美玲. 氟桂利嗪联合银杏达莫治疗老年眩晕的疗效及临床应用. 昆明医科大学学报. 2022(07): 116-120 .  百度学术
百度学术15. 钟文华,刘云,温俊威,吴超,洪云,王林,李曙. 简易密封盒建立人脐静脉血管内皮细胞缺氧/复氧损伤模型. 皖南医学院学报. 2022(04): 307-310 .  百度学术
百度学术16. 朱莹,陈达鑫,王美玲,林珊. 泥胡菜不同极性溶剂萃取物中总酚和总黄酮含量及抗氧化活性测定. 福建中医药. 2022(11): 42-45 .  百度学术
百度学术其他类型引用(10)
-





 下载:
下载:


