-
三尖瓣反流表现为三尖瓣或三尖瓣环结构上的异常,导致一部分血流从右心室反流回右心房,通常由原发性或肺动脉高压、房颤、左心瓣膜疾病导致的继发性功能障碍所致[1]。手术是目前治疗三尖瓣重度反流的最佳选择[2]。胃肠功能障碍是心胸外科手术患者术后常见并发症,且早期胃肠功能障碍患者更容易出现术后机械通气时间延长、重症监护室(ICU)住院时间延长等问题[3]。胃肠动力药是促进患者术后胃肠功能恢复的常见用药,能有效缓解患者术后消化功能紊乱症状。笔者选择2011年1月至2021年12月海军军医大学第一附属医院心血管外科收治的184例三尖瓣重度反流患者,观察并分析术后3 d内预防性使用胃肠动力药在体外循环下三尖瓣置换术患者的临床治疗效果,现报告如下。
-
本研究为回顾性分析,纳入对象为2011年1月至2021年12月于我院收治的重度三尖瓣反流患者。纳入标准:①患者临床诊断为重度三尖瓣反流;②患者接受体外循环下三尖瓣置换手术。排除标准:①手术后3 d内死亡患者;②手术后3 d内出现消化道症状的患者。共收集符合纳入标准的重度三尖瓣反流患者184人,其中,男性患者76例(40.98%),中位年龄54.0[47.0,66.0]岁,女性患者108例(59.02%),中位年龄60.0[52.0,66.0]岁。
-
患者入院后,行术前常规检查。对符合手术指征且有手术意愿的患者采用胸部正中切口或右胸外侧切口进行手术。手术过程中对患者建立体外循环,行生物瓣或机械瓣置换术。术后于我院心外科ICU进行进一步治疗。
-
收集患者的人口统计学资料,包括年龄、性别、疾病史等,术后3 d内胃肠动力药服用情况,术后首次排便时间,手术3 d后胃肠道相关症状,手术3 d后急性肾衰竭、肺部感染、脑卒中等并发症发生情况。此外,收集并记录患者ICU住院时间、机械通气时间、胃管置入时间。
-
术后3 d内服用胃肠动力药定义为预防组,术后3 d内未服用胃肠动力药定义为对照组。排便延迟判定:术后3 d内(包括第3天)排便为正常排便,术后3 d以上排便为排便延迟。
-
采用SPSS 21.0 统计学软件进行数据统计分析。符合正态分布的计量资料采用t检验进行统计,以(
$\bar x $ ±s)表示;不符合正态分布的计量资料采用非参数分析进行统计,以中位数(四分位数间距)[M(QL ~ QU)]表示。计数资料采用卡方(χ2)检验进行统计,以例数(百分比)[n (%)]表示。P<0.05表示差异具有统计学意义。 -
在纳入研究的184例重度三尖瓣反流患者中,有101例患者(54.89%)术后3 d服用胃肠动力药,其中,72例患者(39.13%)术后服用莫沙必利,36例患者(19.57%)术后服用多潘立酮,7例患者(3.80%)同时服用莫沙必利和多潘立酮;83例患者(45.11%)术后3 d内未服用胃肠动力药。两组患者在年龄、性别、BMI、疾病史、手术史均无统计学差异(P>0.05),见表1。
表 1 两组患者一般资料比较
项目 预防组 对照组 χ2(Z)值 P值 年龄 (岁) 56.0 [51.0,67.0] 59.0[49.0,65.0] −0.039 0.970 男性[n (%)] 40 (39.6) 36 (43.4) 0.267 0.653 BMI (kg/m2) 22.5 [20.4,24.0] 21.7 [19.0,23.9] −1.744 0.081 糖尿病[n (%)] 8 (7.9) 6 (7.2) 0.031 1.000 高血压[n (%)] 12 (11.9) 8 (9.6) 0.237 0.645 肝硬化[n (%)] 3 (3.0) 4 (4.8) 0.426 0.703 肾功能不全[n (%)] 3 (3.0) 1 (1.2) 0.668 0.628 脑卒中史[n (%)] 5 (5.0) 8 (9.6) 1.525 0.256 心脏手术史[n (%)] 79 (78.2) 57 (68.7) 2.152 0.177 -
预防组患者术后平均首次排便时间为3.32 d,低于对照组患者术后平均首次排便时间4.67 d。预防组患者中排便延迟的发生率为40.1%,显著低于对照组患者排便延迟发生率65.1%,差异均具有统计学意义(P<0.05),见表2。
表 2 两组患者首次排便时间比较
项目 预防组 对照组 χ2(Z)值 P值 排便时间 (t/d) 3.0[2.0,4.0]*** 4.0[3.0,5.0] −3.634 <0.001 排便延迟[n (%)] 41 (40.6)** 54 (65.1) 10.920 0.001 **P<0.01,***P<0.001,与对照组比较。 -
预防组患者腹胀症状发生率明显低于对照组患者,差异具有统计学意义(P<0.05),其他胃肠功能障碍未见统计学差异(P>0.05),见表3。
表 3 两组患者胃肠功能障碍发生情况比较
项目 预防组[n (%)] 对照组[n (%)] χ2(Z)值 P值 恶心 11 (10.9) 10 (12.0) 0.060 0.820 呕吐 9 (17.8) 5 (6.0) 0.540 0.581 腹胀 2 (2.0)* 8 (9.6) 5.199 0.045 腹泻 3 (3.0) 6 (7.2) 1.776 0.303 消化道出血 4 (4.0) 3 (3.6) 0.015 1.000 *P<0.05,与对照组比较。 -
预防组患者肺部感染发生率显著低于对照组患者(P<0.05),其余术后并发症未见统计学差异(P>0.05)。此外,预防组患者ICU时长、气管插管时长、胃管置入时长均短于对照组患者,差异具有统计学意义(P<0.05),见表4。
表 4 两组患者预后及并发症比较
项目 预防组 对照组 χ2(Z)值 P值 死亡[n (%)] 6 (5.9) 9 (10.8) 1.463 0.283 心功能不全[n (%)] 4 (4.0) 3 (3.6) 0.015 1.000 肾衰[n (%)] 5 (5.0) 10 (12.0) 0.080 0.105 肺部感染[n (%)] 5 (5.0)* 12 (14.5) 4.911 0.039 癫痫/脑卒中[n (%)] 3 (3.0) 4 (4.8) 0.426 0.703 ICU时长 (t/h) 100.0[25.5,85.0]* 176.5[43.0,119.0] −2.190 0.028 气管插管时长 (t/h) 41.0[7.0,21.5]** 126.0[15.0,44.0] −3.127 0.002 胃管置入时长(t/h) 67.0[10.5,26.0]** 143.0[17.0,82.0] −3.191 0.001 *P<0.05,**P<0.01,与对照组比较。 -
重度三尖瓣反流患者常伴有严重的右心衰竭,可能引起患者内脏静脉压长期升高,从而导致患者肠细胞长期缺血和肠屏障功能的破坏[4]。此外,肠黏膜血流在正常生理条件下为黏膜细胞提供足够的氧气和营养,以维持正常的消化功能,而在体外循环的条件下,例如手术后,可能会出现肠黏膜缺血和再灌注损伤,引起患者肠通透性增加和屏障功能受损,导致胃肠蠕动功能降低[5-7]。在本研究中,肠功能紊乱可能是接受体外循环下三尖瓣置换手术患者排便延迟的重要原因。术后胃肠功能障碍增加了住院时间、护理成本和术后发病率。因此,对于体外循环下三尖瓣置换术患者术后应进行早期胃肠功能干预。
本研究排除了手术后3 d内发生消化道症状的患者。这些患者在发生不良反应后通常采用多种手段辅助治疗,这可能会影响对胃肠动力药预防效果的判断,故不纳入本研究。胃肠促动药能够加强胃肠蠕动,促进胃排空,协调胃肠运动,主要用于治疗胃肠道疾病,如功能性消化不良,胃食管反流病,糖尿病性胃轻瘫和术后肠梗阻[8]。本研究中选用莫沙必利和或多潘立酮作为胃肠动力药给药方案,其中莫沙必利给药剂量为5 mg,每日3次;多潘立酮给药剂量为10 mg,每日3次。莫沙必利是一种选择性5-HT4受体激动剂,通过兴奋胃肠道5-HT4受体,从而增加乙酰胆碱的释放,促进患者胃肠道蠕动和排空[9]。多潘立酮是一种多巴胺受体拮抗剂,由于其对胃和小肠的化学感受器触发区和运动功能的影响,常被充当为止吐剂和胃肠促动力剂[10]。同莫沙必利或多潘立酮单独使用相比,二者联合应用有助于患者术后胃肠功能的早期恢复,但可能会增加患者腹泻风险[11]。本研究表明,胃肠动力药在术后3 d内预防性使用,能有效促进三尖瓣置换术后患者的排便,降低排便延迟的发生率。合理的术前生活方式和饮食措施、术后胸段硬膜外镇痛、水电解质平衡、口香糖咀嚼、预防性使用泻药也可作为预防术后排便延迟的有效措施[12, 13]。对于已经出现排便延迟的患者,渗透性或黏液性泻药、促动力药物和维持水电解质平衡等干预措施对缓解症状具有重要意义[14]。
在危重患者的管理中,胃肠动力障碍会继发许多并发症,如反流或误吸导致肺功能降低和呼吸机相关性肺炎、营养不良、败血症等[15]。本研究发现,预防性服用胃肠动力药能有效降低三尖瓣置换术患者术后肺部感染的发生率,并降低术后ICU、机械通气和胃管置入的时间。目前,有研究表明莫沙必利对胃造瘘术患者预防肺炎的有益作用[16]。此外,定期给予多潘立酮可降低急性缺血性卒中患者吸入性肺炎的发生率,缩短住院时间,改善短期临床结局[17]。因此,莫沙必利和多潘立酮等胃肠动力药的促动力作用在三尖瓣术后患者中预防吸入性肺炎方面可能扮演重要作用,值得临床推广和使用。
Observation of the prophylactic use of prokinetic agents in patients after tricuspid valve replacement under cardiopulmonary bypass
-
摘要:
目的 对体外循环下行三尖瓣置换术后患者服用胃肠动力药的治疗效果进行临床分析。 方法 选取2010年6月至2021年12月在海军军医大学第一附属医院心血管外科接受体外循环下三尖瓣置换术的患者作为研究对象,收集并回顾性分析术后3 d内,服用胃肠动力药(预防组)与未服用胃肠动力药(对照组)患者的基线资料、术后首次排便时间和术后恢复情况。 结果 筛选患者184例,其中,预防组101例,对照组83例。预防组患者首次排便时间明显早于对照组患者排便时间(P<0.05),预防组患者腹胀、肺部感染的概率明显低于对照组患者,且预防组患者ICU时长、术后机械通气时长、胃管置入时长明显短于对照组患者(P<0.05)。 结论 术后3 d内服用胃肠动力药能有效改善体外循环下三尖瓣置换术患者预后。 Abstract:Objective To analyze the postoperative therapeutic effect of prokinetic agents in patients after tricuspid valve replacement (TVR) under cardiopulmonary bypass. Methods Patients received TVR under cardiopulmonary bypass (during June 2010 to December 2021) in the department of Cardiovascular Surgery of the First Affiliated Hospital of Naval Medical University were selected as the subjects of our study. The data of basic characteristics, first postoperative defecation time and postoperative recovery condition were collected and retrospectively analyzed in the patients taking prokinetic agents within three days after surgery (prevention group) and patients not taking prokinetic agents within three days after surgery (control group). Results A total of 184 patients were selected, including 101 in the prevention group and 83 in the control group. The first defecation time of patients in the prevention group was significantly earlier than that in the control group (P<0.05). The incidences of abdominal distension and pulmonary infection in the prevention group were significantly lower than that in the control group. The length of time in ICU, postoperative mechanical ventilation and nasogastric tube decompression in the prevention group were significantly shorter than that in the control group (P<0.05). Conclusion Taking prokinetic agents within three days after TVR under cardiopulmonary bypass could effectively improve the prognosis of patients. -
Key words:
- prokinetic agents /
- tricuspid valve replacement /
- clinical effect /
- retrospective study
-
口腔溃疡膜是海军军医大学附属长征医院的特色院内制剂,该制剂主要由克霉唑、硫酸新霉素、冰片、盐酸达克罗宁、地塞米松磷酸钠等成分组成,呈微黄色至淡黄色半透明膜。临床用于治疗多发性口腔溃疡。溃疡是口腔疾病的常见表现,口腔黏膜溃疡病因可分为4类:感染性、免疫性、外伤性和肿瘤性[1]。地塞米松磷酸钠属糖皮质激素,经常用于加速溃疡愈合、减轻口腔溃疡的局部症状[2];克霉唑是一种常用于治疗真菌感染的抗真菌药物[3]。口腔溃疡膜能保护局部溃疡面,延长局部作用时间、提高药物浓度,具有定位释放、使用方便等优点[4]。本制剂室唐蕾等[5]通过测定口腔溃疡膜中克霉唑和地塞米松磷酸钠的含量建立了一套操作简单、准确性好的HPLC含量测定方法,适用于口腔溃疡膜的质量标准控制。但随着制剂标准的提高,在《军队医疗机构制剂许可证》验收细则中明确规定:配制制剂的原料药应符合法定药品标准,辅料及直接接触制剂的包装材料应符合法定标准。因此,一些原料药及辅料在更换药用标准后,按照原先的样品前处理方法测得的含量一直偏低。本文以口腔溃疡膜中主要有效成分地塞米松磷酸钠和克霉唑的含量为指标,对口腔溃疡膜中有效成分的提取工艺进行研究,并进一步优化地塞米松磷酸钠和克霉唑的含量测定方法。
1. 仪器和试药
1.1 仪器
Agilent 1260型高效液相色谱仪(美国Agilent公司):包含G7104C(四元泵)输液泵,G7129C自动进样器,G7116A柱温箱,G7115A DAD检测器;色谱柱为Agilent Zobax SB-C18柱(250 mm×4.6 mm,5 μm,美国Agilent公司);Sartorius 天平(型号:BSA124S-CW,十万分之一天平,赛多利斯科学仪器有限公司);超声仪(SK7200H型,上海科导超声仪器有限公司);Eppendorf移液器(德国);WL-901 Vortex旋涡振荡混和器(海门市其林贝尔仪器制造有限公司)。
1.2 试剂与药品
地塞米松磷酸钠对照品(批号:ZN1107XA)、克霉唑对照品(批号:H01S9Z68980),购自上海源叶生物科技有限公司;甲醇(色谱纯,德国Fisher公司);娃哈哈纯净水(纯净水,杭州娃哈哈集团有限公司);磷酸二氢钾等其余试剂均为分析纯。口腔溃疡膜(批号:190919、190923、190926,每片含地塞米松磷酸钠0.4 mg,克霉唑6.53 mg,海军军医大学附属长征医院制剂中心自制)。
2. 方法与结果
2.1 色谱条件
色谱柱:Agilent Zobax SB-C18柱(250 mm×4.6 mm,5 μm);流动相:甲醇−0.05 mol/L磷酸二氢钾溶液(70∶30, 用磷酸溶液调pH值4.4~4.5);紫外检测波长:230 nm;流速:1.0 ml/min;柱温:30 ℃;采集时间:30 min,进样量:20 μl。
2.2 溶液的制备
2.2.1 对照品溶液
精密称取地塞米松磷酸钠16.328 mg置于10 ml量瓶中,加甲醇-水(7∶3)溶解并稀释至刻度,摇匀,得浓度为1.632 8 mg/ml的地塞米松磷酸钠对照品储备液。精密称取克霉唑对照品20.058 mg置于10 ml量瓶中,加甲醇-水(7∶3)溶解并稀释至刻度,摇匀,得浓度为2.005 8 mg/ml的克霉唑对照品储备液。
2.2.2 混合对照品溶液
分别精密量取地塞米松磷酸钠、克霉唑对照品储备液适量,加甲醇-水(7∶3)配制成含地塞米松磷酸钠16.328 μg/ml和克霉唑200.58 μg/ml的混合对照品溶液。
2.2.3 供试品溶液
取口腔溃疡膜剪成3~5 mm大小的碎片,精密称取样品0.2 g,置于100 ml容量瓶中,加入30 ml水,超声30 min,取出,放冷,加入甲醇并稀释至刻度,摇匀,即得。
2.2.4 阴性对照品溶液
参照本课题组前期实验方法,制备阴性对照品溶液[5]。
2.3 方法学考察
2.3.1 专属性试验
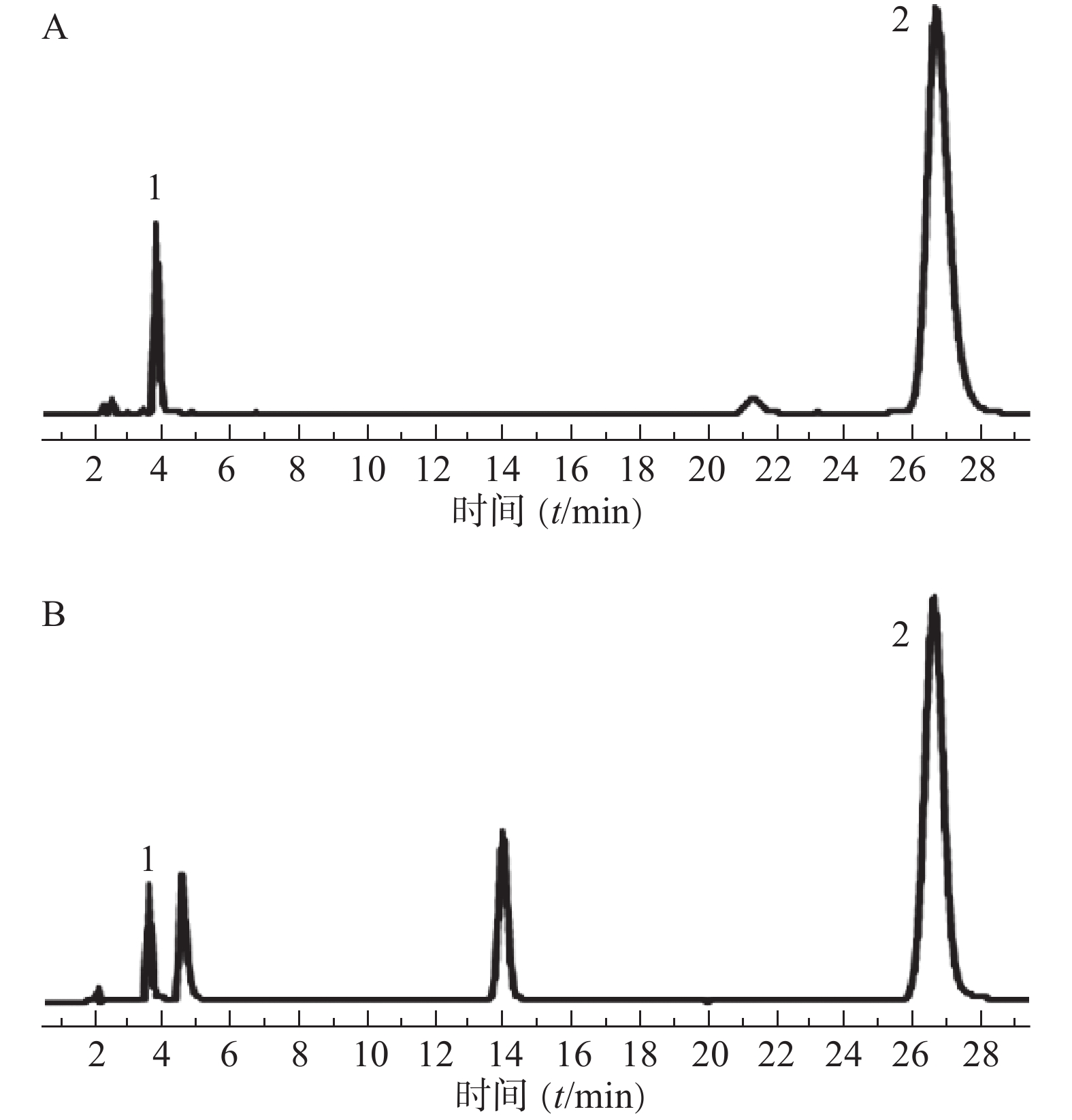
分别取混合对照品溶液(地塞米松磷酸钠、克霉唑)和供试品溶液,按“2.1”项下色谱条件测定,记录色谱图,结果见图1。图中显示供试品溶液中地塞米松磷酸钠和克霉唑保留时间与对照品溶液相应色谱峰的保留时间一致。地塞米松磷酸钠和克霉唑与其相近的其他峰分离完全(分离度>1.5),即本试验条件下地塞米松磷酸钠和克霉唑与其他组分分离完全。
2.3.2 线性关系的考察
精密量取“2.2.2”项下混合对照品溶液适量,稀释成以下浓度的混合对照品溶液:地塞米松磷酸钠0.482 0、0.816 4、1.632 8、4.082 0、8.164 0、16.328 0 μg/ml;克霉唑5.014 5、10.029 0、20.058 0、50.14 50、100.290 0、200.580 0 μg/ml,按“2.1”项下色谱条件进行测定,并记录色谱峰面积。以峰面积为纵坐标(Y),对照品质量浓度为横坐标(C),绘制标准曲线,并进行线性回归,结果见表1。
表 1 地塞米松磷酸钠和克霉唑的线性关系考察成分 回归方程 r 线性范围(μg/ml) 地塞米松磷酸钠 Y=34.961C+27.986 0.999 9 0.482 0~16.328 0 克霉唑 Y=32.366C+24.092 0.999 8 5.014 5~200.580 0 2.3.3 精密度试验
取同一批口腔溃疡膜(批号:190919),按“2.2.3”项方法制备供试品溶液,按“2.1”项色谱条件进行测定,连续进样6次,记录峰面积。计算地塞米松磷酸钠和克霉唑峰面积RSD分别为0.65%和0.33%,表明仪器精密度良好。
2.3.4 重复性试验
取同一批口腔溃疡膜(批号:190919),按“2.2.3”项方法平行制备6份供试品溶液,按“2.1”项色谱条件进行测定,记录峰面积。计算地塞米松磷酸钠和克霉唑峰面积RSD分别为0.56%和0.54%,表明该方法重复性良好。
2.3.5 稳定性试验
取同一批口腔溃疡膜(批号:190919),按“2.2.3”项方法制备供试品溶液,按“2.1”项色谱条件,分别在0、2、4、6、12、24 h进样测定,记录峰面积。计算地塞米松磷酸钠和克霉唑峰面积RSD值分别为0.94%和1.33%,表明供试品溶液在室温放置24 h内稳定性良好。
2.3.6 加样回收率试验
精密称取已知含量的样品(批号:190919)0.2 g,共6份,置于100 ml容量瓶中,加入各对照品适量,按“2.2.3”项方法制备供试品溶液,按“2.1”项色谱条件进样测定,记录峰面积,计算加样回收率。结果地塞米松磷酸钠和克霉唑的平均加样回收率分别为(103.97±1.02)%和(104.23±0.63)%,表明本法回收率良好。
2.3.7 样品含量测定
取3批口腔溃疡膜,按“2.2.3”项方法制备供试品溶液,按“2.1”项色谱条件进行测定,计算样品中地塞米松磷酸钠和克霉唑的含量,结果见表2。
表 2 口腔溃疡膜中地塞米松磷酸钠和克霉唑的含量测定结果(n=3,$\bar x$ ±s)批号 含量[标示量(%)] 地塞米松磷酸钠 克霉唑 190919 76.600 0±0.005 2 86.800 0±0.011 3 190923 85.900 0±0.011 5 99.100 0±0.025 9 190926 74.900 0±0.043 7 85.700 0 ±0.067 6 3. 讨论
3.1 提取方法的优化
本研究根据口腔溃疡膜的特性,对溶剂种类、溶剂提取顺序进行考察,由于口腔溃疡膜中含羧甲基纤维素钠,这是由一种天然纤维素衍生的阴离子水溶性聚合物[6],易溶于水,因此需要一定比例的水将膜剂破坏,才能释放出膜剂中的有效成分地塞米松磷酸钠和克霉唑。
3.1.1 甲醇超声提取
取口腔溃疡膜剪成3~5 mm大小的碎片,精密称取样品0.2 g,置于100 ml容量瓶中,加入甲醇35 ml,超声30 min,取出,放冷,加入15 ml水,混匀后用甲醇-水(7∶3)定容,摇匀,即得。
3.1.2 水超声提取
取口腔溃疡膜剪成3~5 mm大小的碎片,精密称取样品0.2 g,置于100 ml容量瓶中,加入30 ml水,超声30 min,取出,放冷,加入甲醇并稀释至刻度,摇匀,即得。
3.1.3 以70%甲醇超声提取
取口腔溃疡膜剪成3~5 mm大小的碎片,精密称取样品0.2 g,置于100 ml容量瓶中,加入甲醇-水(7∶3)30 ml,超声30 min,取出,放冷,加入甲醇-水(7∶3)稀释至刻度,摇匀,即得。
用以上不同溶剂提取口腔溃疡膜,每份样品、每种溶剂平行提取3次,按“2.1”项所述色谱条件测定地塞米松磷酸钠和克霉唑含量,结果见表3。实验结果显示:水超声提取和70%甲醇超声提取对口腔溃疡膜中有效成分的提取效果相当,但水超声提取相对简单,故选用水超声提取30 min为最佳提取工艺。
3.2 流动相pH的优化
在液相色谱条件优化实验中,比较了不同pH时的采集时间,结果发现:pH在4.4~4.5时采集时间为30 min,较之于前缩短了5 min,方法更便捷。
表 3 不同溶剂对口腔溃疡膜有效成分提取率的影响[n=3,实测值/标示量(%)]提取方法 地塞米松磷酸钠 克霉唑 甲醇超声提取 67.46 74.49 71.58 79.06 73.09 72.64 水超声提取 108.29 101.28 104.08 101.03 105.88 103.38 70%甲醇超声提取 104.27 95.00 109.52 100.52 106.89 103.54 本研究基于HPLC同时测定口腔溃疡膜中地塞米松磷酸钠、克霉唑含量的方法,经提取工艺的优化和全面的方法学考察,成功用于测定样品中地塞米松磷酸钠和克霉唑的含量,该法简便可靠,可为口腔溃疡膜的质量控制提供依据,也为其质量标准研究奠定了基础。
-
表 1 两组患者一般资料比较
项目 预防组 对照组 χ2(Z)值 P值 年龄 (岁) 56.0 [51.0,67.0] 59.0[49.0,65.0] −0.039 0.970 男性[n (%)] 40 (39.6) 36 (43.4) 0.267 0.653 BMI (kg/m2) 22.5 [20.4,24.0] 21.7 [19.0,23.9] −1.744 0.081 糖尿病[n (%)] 8 (7.9) 6 (7.2) 0.031 1.000 高血压[n (%)] 12 (11.9) 8 (9.6) 0.237 0.645 肝硬化[n (%)] 3 (3.0) 4 (4.8) 0.426 0.703 肾功能不全[n (%)] 3 (3.0) 1 (1.2) 0.668 0.628 脑卒中史[n (%)] 5 (5.0) 8 (9.6) 1.525 0.256 心脏手术史[n (%)] 79 (78.2) 57 (68.7) 2.152 0.177 表 2 两组患者首次排便时间比较
项目 预防组 对照组 χ2(Z)值 P值 排便时间 (t/d) 3.0[2.0,4.0]*** 4.0[3.0,5.0] −3.634 <0.001 排便延迟[n (%)] 41 (40.6)** 54 (65.1) 10.920 0.001 **P<0.01,***P<0.001,与对照组比较。 表 3 两组患者胃肠功能障碍发生情况比较
项目 预防组[n (%)] 对照组[n (%)] χ2(Z)值 P值 恶心 11 (10.9) 10 (12.0) 0.060 0.820 呕吐 9 (17.8) 5 (6.0) 0.540 0.581 腹胀 2 (2.0)* 8 (9.6) 5.199 0.045 腹泻 3 (3.0) 6 (7.2) 1.776 0.303 消化道出血 4 (4.0) 3 (3.6) 0.015 1.000 *P<0.05,与对照组比较。 表 4 两组患者预后及并发症比较
项目 预防组 对照组 χ2(Z)值 P值 死亡[n (%)] 6 (5.9) 9 (10.8) 1.463 0.283 心功能不全[n (%)] 4 (4.0) 3 (3.6) 0.015 1.000 肾衰[n (%)] 5 (5.0) 10 (12.0) 0.080 0.105 肺部感染[n (%)] 5 (5.0)* 12 (14.5) 4.911 0.039 癫痫/脑卒中[n (%)] 3 (3.0) 4 (4.8) 0.426 0.703 ICU时长 (t/h) 100.0[25.5,85.0]* 176.5[43.0,119.0] −2.190 0.028 气管插管时长 (t/h) 41.0[7.0,21.5]** 126.0[15.0,44.0] −3.127 0.002 胃管置入时长(t/h) 67.0[10.5,26.0]** 143.0[17.0,82.0] −3.191 0.001 *P<0.05,**P<0.01,与对照组比较。 -
[1] ANTUNES M J, RODRÍGUEZ-PALOMARES J, PRENDERGAST B, et al. Management of tricuspid valve regurgitation: position statement of the European Society of Cardiology Working Groups of Cardiovascular Surgery and Valvular Heart Disease[J]. Eur J Cardiothorac Surg, 2017, 52(6): 1022-1030. doi: 10.1093/ejcts/ezx279 [2] Correction to: 2020 ACC/AHA guideline on the management of patients with valvular heart disease: executive summary: a report of the American college of cardiology/American heart association task force on clinical practice guidelines[J]. Circulation, 2021, 143(5): e228. [3] SEILITZ J, EDSTRÖM M, SKÖLDBERG M, et al. Early onset of postoperative gastrointestinal dysfunction is associated with unfavorable outcome in cardiac surgery: a prospective observational study[J]. J Intensive Care Med, 2021, 36(11): 1264-1271. doi: 10.1177/0885066620946006 [4] POLSINELLI V B, MARTEAU L, SHAH S J. The role of splanchnic congestion and the intestinal microenvironment in the pathogenesis of advanced heart failure[J]. Curr Opin Support Palliat Care, 2019, 13(1): 24-30. doi: 10.1097/SPC.0000000000000414 [5] KAWANO S, TSUJI S. Role of mucosal blood flow: a conceptional review in gastric mucosal injury and protection[J]. J Gastroenterol Hepatol, 2000, 15Suppl:: D1-6. [6] BRAUN J P, SCHROEDER T, BUEHNER S, et al. Splanchnic oxygen transport, hepatic function and gastrointestinal barrier after normothermic cardiopulmonary bypass[J]. Acta Anaesthesiol Scand, 2004, 48(6): 697-703. doi: 10.1111/j.1399-6576.2004.00392.x [7] WANG Y B, LIU J, YANG Z X. Effects of intestinal mucosal blood flow and motility on intestinal mucosa[J]. World J Gastroenterol, 2011, 17(5): 657-661. doi: 10.3748/wjg.v17.i5.657 [8] HIYAMA T, YOSHIHARA M, TANAKA S, et al. Effectiveness of prokinetic agents against diseases external to the gastrointestinal tract[J]. J Gastroenterol Hepatol, 2009, 24(4): 537-546. doi: 10.1111/j.1440-1746.2009.05780.x [9] CURRAN M P, ROBINSON D M. Mosapride in gastrointestinal disorders[J]. Drugs, 2008, 68(7): 981-991. doi: 10.2165/00003495-200868070-00007 [10] CAMILLERI M, ATIEH J. New developments in prokinetic therapy for gastric motility disorders[J]. Front Pharmacol, 2021, 12: 711500. doi: 10.3389/fphar.2021.711500 [11] 王瑶, 于玲, 曹文文. 莫沙必利联合多潘立酮对肠内营养期结直肠癌患者胃肠功能的影响[J]. 现代消化及介入诊疗, 2019, 24(4): 347-351. [12] BRAGG D, EL-SHARKAWY A M, PSALTIS E, et al. Posto-perative ileus: recent developments in pathophysiology and management[J]. Clin Nutr, 2015, 34(3): 367-376. doi: 10.1016/j.clnu.2015.01.016 [13] DE AZEVEDO R P, FREITAS F G R, FERREIRA E M, et al. Daily laxative therapy reduces organ dysfunction in mechanically ventilated patients: a phase II randomized controlled trial[J]. Crit Care, 2015, 19(1): 329. doi: 10.1186/s13054-015-1047-x [14] CHOR C Y T, MAHMOOD S, KHAN I H, et al. Gastrointestinal complications following cardiac surgery[J]. Asian Cardiovasc Thorac Ann, 2020, 28(9): 621-632. doi: 10.1177/0218492320949084 [15] CHAPMAN M J, NGUYEN N Q, DEANE A M. Gastrointestinal dysmotility: clinical consequences and management of the critically ill patient[J]. Gastroenterol Clin North Am, 2011, 40(4): 725-739. doi: 10.1016/j.gtc.2011.09.003 [16] TAKATORI K, YOSHIDA R, HORAI A, et al. Therapeutic effects of mosapride citrate and lansoprazole for prevention of aspiration pneumonia in patients receiving gastrostomy feeding[J]. J Gastroenterol, 2013, 48(10): 1105-1110. doi: 10.1007/s00535-012-0725-6 [17] ALLAMI A, KIANIMAJD S, MAVANDADI S, et al. Evaluation of domperidone efficacy to prevent aspiration pneumonia in patients with acute ischemic stroke: a randomized clinical trial[J]. Acta Neurol Belg, 2022, 122(5): 1337-1342. doi: 10.1007/s13760-022-01925-0 -





 下载:
下载:

 下载:
下载: 


