-
随着放射诊断技术与介入治疗手段的发展,造影剂的使用越来越广泛。相对的,造影剂所引起的急性肾功能损伤也日益受到临床关注。造影剂肾病(contrast-induced nephropathy, CIN)是接受冠状动脉造影或经皮冠状动脉腔内成形术(percutaneous transluminal coronary angioplasty, PTCA)后常见的不良后果[1]。由于涉及多种危险因素,CIN发病率为0%~24%不等[2]。临床因血管疾病而接受造影的患者,通常合并高血压。《2018美国放射协会手册》指出需要药物治疗的高血压病史且为造影剂肾病的危险因素之一,可能需要在使用碘造影剂前进行肾功能的评估[3]。但降压药物对肾功能具体的影响以及造影术前是否需要停用这些药物还未得到严格的证实。近年来,肾素-血管紧张素-醛固酮系统抑制剂(renin-angiotensin-aldosterone system inhibitors,RAASi)包括血管紧张素转化酶抑制剂(angiotensin convening enzyme inhibitor, ACEI)和血管紧张素受体拮抗剂(angiotensin receptor blockers, ARB)对造影剂急性肾损的影响尚存在争议。一项纳入12篇文献包含4 493名患者的meta分析发现,在接受RAASi和未接受RAASi治疗的患者之间,CIN的发生率没有差异[4],反而术前接受RAASi可降低造影剂急性肾损伤的发生率和医院病死率[5],但也有部分学者认为ACEI/ARB会增加CIN的发生率[6-7]。β受体阻滞剂作为危险因素常被认为与造影剂的过敏样反应相关[3, 8],而对肾功能的影响鲜有研究。另外,在造影前使用CCB类的降压药物预防CIN的作用也存在争议[9],还需进一步考察。本研究回顾分析了常见抗高血压药物对PTCA术后患者短期肾功能的影响,探讨其对CIN的作用及安全性,以期为临床用药提供更多的循证医学证据。
-
选取2020年1月至2020年12月南京鼓楼医院心血管内科疑似冠心病行冠脉造影术的193例住院患者为研究对象,所有患者在PTCA治疗前后均接受了标准水化治疗。纳入标准:①年龄在18周岁以上。②冠脉造影后行PTCA术的患者。③术前均规律(≥7 d)服用ACEI/ARB、β受体阻滞剂或CCB类药物。排除标准:①同时服用两种及以上降压药的患者。②术前术中使用袢利尿剂患者。③碘过敏试验阳性或2周内静脉使用过对比剂。④严重肾功能不全:eGFR<30 ml/(min·1.73 m2)。⑤存在其他导致急性肾功能损伤的病因(如使用肾毒性药物、慢性肾功能不全、血容量不足、心力衰竭)。⑥患有自身免疫性疾病、严重感染及肿瘤者。试验分组:根据时间顺序依次纳入,分为4组,不服用降压药物或至少停药2周的单纯水化组(50例)、ACEI/ARB组(50例)、β受体阻滞剂组(47例)、CCB组(46例)。
-
冠脉造影及介入治疗通过有经验的心内科介入医师在标准程序下完成,所有患者均使用碘海醇为造影剂。回顾性收集患者的临床资料,包括患者的年龄、性别、体重、身高、血压、血脂、血糖、尿酸、造影剂用量、造影前及造影48 h后的血肌酐(Scr)、尿素氮(BUN)、Cockcroft-Gault法计算肌酐清除率(Ccr)、MDRD法计算肾小球滤过率(eGFR)。CIN诊断标准[10-11]为:排除其他影响肾功能因素,造影暴露后48 h内,SCr水平绝对值增加44.2 μmol/L或超过基础值25%以上。所有患者在造影前静脉滴注0.9%氯化钠注射液250 ml进行水化治疗。
-
数据采用SPSS 22.0统计学软件进行分析。计量资料用(
$\bar x$ ±s)表示。统计指标均进行正态性及方差齐性检验,造影前后连续变量的比较采用配对t检验。多组间连续变量的比较采用单因素方差分析,方差齐采用LSD检定,方差不齐采用Games-Howell检验。计数资料采用Fisher确切概率法,用[n(%)]表示。所有统计分析,以P<0.05表示数据存在差异,具有统计学意义。 -
本研究一共纳入193例患者,如表1所示,4组患者在年龄、性别、BMI、血压、血脂、血糖、尿酸、造影剂用量以及基础肾功能指标等方面,差异均无统计学意义(P>0.05)。
表 1 4组患者基本资料比较[n(%),
$\bar x$ ±s]组别 年龄(岁) 男性 BMI(kg/m2) 收缩压
(mmHg)舒张压
(mmHg)TC
(mmol/L)TG
(mmol/L)HDL-C
(mmol/L)LDL-C
(mmol/L)单纯水化组(n=50) 60.58±11.35 28(56) 23.96±2.91 130.62±16.99 79.98±13.04 4.48±0.91 1.43±0.84 1.26±0.34 2.55±0.71 β-受体阻滞剂组(n=47) 64.40±11.61 32(68) 25.13±3.60 125.79±15.93 74.89±13.19 4.03±0.99 1.50±0.91 1.09±0.35 2.30±082 ACEI/ARB组(n=50) 65.04±6.52 25(50) 24.37±3.05 134.86±17.17 76.52±10.29 4.15±0.97 1.60±0.91 1.16±0.30 2.28±0.80 CCB组(n=46) 65.67±9.25 26(57) 24.45±2.81 139.43±14.57 78.91±9.28 4.23±0.87 1.34±0.61 1.20±0.30 2.38±0.74 组别 UA(μmol/L) FBG
(mmol/L)造影剂用量(ml) Scr
(μmol/L)BUN
(mmol/L)eGFR[ml/
(min·1.73 m2)]eGFR>90 [ml/
(min·1.73 m2)]eGFR<60 [ml/
(min·1.73 m2)]Ccr
(ml/min)单纯水化组(n=50) 330.48±82.36 5.35±1.06 122.32±56.11 63.62±16.01 5.25±1.17 112.04±27.17 11(22) 1(2) 97.86±29.83 β-受体阻滞剂组(n=47) 378.19±87.31 5.32±1.87 124.83±60.38 66.30±14.61 5.32±1.48 107.05±19.59 8(17) 1(2) 95.88±26.84 CEI/ARB组(n=50) 363.88±98.07 5.50±1.25 121.79±59.22 64.94±12.69 5.48±1.30 103.26±20.23 12(24) 1(2) 89.91±23.94 CCB组(n=46) 343.87±81.79 5.40±1.58 126.48±58.76 63.57±13.90 5.51±1.34 106.93±20.12 8(17) 1(2) 91.98±28.75 -
应用造影剂48 h后肾功能指标变化如表2所示。CIN发生率为0%,4组患者的Ccr在手术前后均无变化,组间也无差异。除了单纯水化组,服用抗高血压药物组BUN皆有一定幅度的下降,其中,β受体阻滞剂组术后与术前相比具有显著差异。并且,β受体阻滞剂组术后BUN水平与单纯水化组、CCB组之间也存在组间差异。另外,与术前相比,β受体阻滞剂组患者的eGFR水平在术后也显著降低。差异具有统计学意义(P<0.05)。
表 2 4组患者造影前后肾功能指标的比较
组别 Scr(μmol/L) BUN(mmol/L) eGFR[ml/(min·1.73 m2)] Ccr(ml/min) 术前 术后48 h 术前 术后48 h 术前 术后48 h 术前 术后48 h 单纯水化组(n=50) 63.62±16.01 64.04±16.66 5.25±1.17 5.34±1.33 112.04±27.17 110.27±25.58 97.86±29.83 97.42±30.39 β受体阻滞剂组(n=47) 66.30±14.61 64.53±14.00 5.32±1.48 4.71±1.01*▲ 107.05±19.59 105.61±18.35▲ 95.88±26.84 98.88±28.55 ACEI/ARB组(n=50) 64.94±12.69 64.98±13.28 5.48±1.30 5.26±1.47 103.26±20.23 103.23±20.29 89.91±23.94 90.02±24.70 CCB组(n=46) 63.57±13.90 63.28±13.27 5.51±1.34 5.42±1.30# 106.93±20.12 111.52±24.62 91.98±28.75 92.20±30.06 *P<0.05,与单纯水化组比较;#P<0.05,与β受体阻滞剂组比较;▲P<0.05,与同组术前比较。 -
将β受体阻滞剂组患者按照血压水平分级,比较不同血压水平下的肾功能情况,结果如表3所示。SBP≥140或DBP≥90的患者在使用造影剂之前,Scr与Ccr水平均显著高于SBP<140且DBP<90的患者(P<0.05)。
表 3 β受体阻滞剂组不同血压水平造影前后肾功能指标的比较
肾功能指标 SBP<140且DBP<90(n=34) SBP≥140或DBP≥90(n=13) 术前 术后48 h 术前 术后48 h Scr(μmol/L) 64.85±11.72 63.28±11.79 70.08±20.49* 67.81±18.78 BUN(mmol/L) 5.31±1.59 4.71±1.05 5.36±1.19 4.71±0.92 eGFR(ml/(min·1.73 m2) 108.58±18.10 105.40±20.44 103.06±23.38 107.77±12.16 Ccr(ml/min) 95.55±23.13 98.53±25.74 96.74±35.91* 99.75±36.06 *P<0.05,与SBP<140且DBP<90组比较。 -
CIN的危险因素有很多,包括:年龄>60岁、肾功能不全、高血压、糖尿病、造影剂剂量大、使用具有肾毒性的药物等[12],其中最危险的因素是存在慢性肾脏病,且疾病发展严重程度与发生CIN风险有关。当eGFR<30 ml/(min·1.73 m2)时,患者CIN发病率是正常人群的3倍[13]。本研究纳入的患者肾功能基础水平均处于正常值,造影前均进行了标准水化治疗,且造影剂用量低于易发生CIN的200 ml[14],又排除了其他对肾功能有影响的药物,因此未观测到CIN的发生。
Scr、BUN、eGFR、Ccr都是常见的用以评价肾功能的指标。其中,Scr受年龄、饮食、肌肉指数等众多因素影响,其浓度上升需要时间且只有在eGFR下降到50%时才升高,因此难以用于早期预测CIN的发生[15]。BUN与Scr相似,灵敏度与特异性较差。除了肾功能之外,BUN的浓度还取决于每日膳食蛋白摄入量、肾血流量、肝功能和患者的水合作用。有趣的是,在本研究中,除了单纯水化组以外,服用抗高血压药的患者在使用造影剂的短期内BUN水平都有轻微幅度的下降,这可能是因为其影响肾功能血流量,导致肾功能短暂性的失调,临床意义不大。在造影前评估基础肾功能损害(主要依靠eGFR)是预测患者发生CIN危险的最重要的标志。本研究中,除了β受体阻滞剂组eGFR水平在造影后有轻微下降,其余ACEI/ARB、CCB组未见明显变化。但β受体阻滞剂组的下降是在正常范围内且β受体阻滞剂作为冠心病患者用来降低心率的基础用药,并不建议术前停用。但对于发生急性肾损伤或eGFR<30 ml/(min·1.73 m2)的患者,在临床可行的情况下,还是应当谨慎去除非必要的潜在肾毒性药物[16]。另外,根据研究结果,应当格外关注那些本身基础血压控制不佳的人群,在确定无CIN发生的前提下,肾功能恢复至基线水平后,再重新启动药物治疗。
此外,作为一项回顾性分析,本研究也存在一定的局限性。①未探讨造影剂对不同肾功能损伤患者的影响。②评估的是短期内肾功能的变化,而未长期动态跟踪造影剂术后一段时间内降压药对肾功能的影响。③CIN的早期预测指标不够全面,目前研究发现的一些更敏感的生物标记物,如肾阻力指数(RRI)、肾损伤分子(KIM-1)、胱抑素C(CysC)可被选择。④未对高血压药物详细再分类,且药物使用周期未进行分层分析,忽略了长期用药对结果可能产生的影响。因此,期待未来有更多前瞻性的、大样本量的研究去进一步指导临床安全用药。
Effects of antihypertensive drugs on renal function after percutaneous transluminal coronary angioplasty
-
摘要:
目的 评估经皮冠状动脉腔内成形术后应用抗高血压药对患者肾功能损伤的影响。 方法 回顾分析2020年1月至2020年12月在南京鼓楼医院心血管内科行经皮冠状动脉腔内成形术治疗并且规律服用抗高血压药物的患者,共193例。根据用药种类不同分为4组:血管紧张素转化酶抑制剂/血管紧张素受体拮抗剂(ACEI/ARB)组、β受体阻滞剂组、钙离子通道阻滞剂(CCB)组、单纯水化组,所有患者围术期均给予常规水化。比较患者手术前后肌酐(Scr)、尿素氮(BUN)、肾小球滤过率(eGFR)、肌酐清除率(Ccr)的水平变化。 结果 4组患者造影剂术后造影剂肾病的发生率为0。与术前相比,4组患者在Scr与Ccr水平上无明显变化,除单纯水化组,其余3组在术后BUN水平降低,其中,β受体阻滞剂组显著降低,且与单纯水化组、CCB组存在统计学差异。此外,β受体阻滞剂组术后eGFR水平也显著降低,其中,血压高值的患者(SBP≥140或DBP≥90)在术前Scr 与Ccr水平即与正常血压者(SBP<140且DBP<90)存在差异。 结论 冠状动脉造影术前使用ACEI/ARB与CCB类抗高血压药对患者短期内肾功能无影响,β受体阻滞剂可能轻微降低肾功能,应对高血压人群特别关注。 -
关键词:
- 经皮冠状动脉腔内成形术 /
- 造影剂肾病 /
- 血管紧张素转化酶抑制剂 /
- 血管紧张素受体拮抗剂 /
- β受体阻滞剂 /
- 钙离子通道阻滞剂
Abstract:Objective To evaluate the effects of antihypertensive drugs on renal function after percutaneous transluminal coronary angioplasty. Methods A retrospective analysis was performed on 193 patients who underwent percutaneous transluminal coronary angioplasty and took antihypertensive drugs regularly. Those patients were admitted to Nanjing Drum Tower Hospital during January 2020 to December 2020. The patients were divided into ACEI/ARB group, β-blockers, calcium channel blockers and hydration control group. All patients received routine hydration during the perioperative period. The changes of serum creatinine (Scr), blood urea nitrogen (BUN), estimated glomerular filtration rate(eGFR) and endogenous creatinine clearance rate (Ccr) before and after operation were compared. Results The incidence of CIN was 0% in four groups. Compared with the preoperative, there was no significant change in Scr and Ccr in every group. Except for the hydration control group, the BUN levels in three treated groups were reduced after postoperative. Specifically, the BUN reduction in β-blockers group has statistically significant difference compared to the hydration control group and CCB group. In addition, eGFR levels were significantly reduced in the β-blockers group. Preoperative Scr and Ccr levels in patients with high blood pressure (SBP≥140 or DBP≥90) were significantly different from the patients with normal blood pressure (SBP<140 and DBP<90). Conclusion The use of ACEI/ARB and CCB before percutaneous transluminal coronary angioplasty had no effect on renal function in the short term. β-blockers can slightly reduce renal function, especially in patients with high blood pressure, who should receive special attention. -
慢性非传染性疾病(NCD)简称慢性病,是心脑血管疾病、肿瘤、糖尿病、慢性呼吸系统疾病、慢性牙病、骨质疏松症、神经精神病、慢性肝肾疾病、慢性骨关节病、良性前列腺肥大和先天异常等疾病的总称[1]。因慢性病死亡的人数占全球死亡人数的60%[2],在我国,慢性病所造成的经济负担占疾病总经济负担的50%以上[3],慢性疾病带来的一系列问题已成为国内外学者关注的重点和难点。作为基层卫生服务的基础,社区在慢性疾病的防控中占据重要地位。然而,目前关于社区慢性病管理的研究虽然多,但结论并不一致,例如,国外研究结果显示该领域的研究主题分布于慢性病患者护理与教育、慢性病管理、慢性病治疗、慢性病患者生命质量评价与管理等部分,而我国的研究主题主要集中在糖尿病和高血压的相关研究[4-5],且随着我国经济的快速发展,国外结论并不能完全适应我国国情。因此,本研究拟借助文献共现分析系统Bicomb2.0软件[6]及常用工具SPSS18,对发表于中国学术期刊网络出版总库中的社区慢性病管理研究文献进行数据挖掘分析,从时间分布、地域分布、机构、作者等内容出发,分析近10年内社区慢性病管理领域的研究现状和热点,以期为我国社区慢性疾病的防控体系提供科学参考和建议。
1. 资料与方法
1.1 数据来源
在中国学术期刊网络出版总库(《中国学术期刊(网络版)》、中国博士学位论文全文数据库、中国优秀硕士学位论文全文数据库)中,以“社区”+“慢性病管理”为主题词进行主题检索,时间限定为2010年1月至2020年1月,收集用于分析的文献资料。根据标题和摘要,排除所有非研究型论文,如综述、进展、会议、访谈、对话、稿约、介绍等。
1.2 研究方法
采用文献计量学分析方法,对纳入的社区慢性病管理研究论文分别从发表时间、地域分布、学术机构、来源期刊、基金类型等方面进行文献计量学分析。运用高频词低频词界分公式,确定出本次统计论文的高频关键词,进而揭示2010—2020年社区慢性病管理研究领域的研究现状与热点。
1.3 统计学方法
选用由中国医科大学崔雷教授研发的文献共现分析系统Bicomb 2.0软件工具和SPSS 18为研究工具,进行统计分析[3]。
2. 结果
2.1 社区慢性病管理研究型论文发表时间分布
2010年1月至2020年1月期间,共计发表相关文献1 427篇,其中,2017—2019年发表文献数量最多,平均每年超过200篇,具体见表1。
表 1 2010—2020年社区慢性病研究型论文发表时间分布情况发表年份 文献数量(篇) 2010 89 2011 104 2012 97 2013 108 2014 116 2015 132 2016 155 2017 216 2018 191 2019 213 2020① 6 总计 1 427 注:“①”表示统计至当年1月。 2.2 社区慢性病管理研究型论文发表地域分布
全部纳入的1 427篇文献中,中文文献1347篇(94.4%),英文文献80篇(5.6%)。其中第一作者单位为美国的29篇,澳大利亚14篇,英国、加拿大各5篇,德国、意大利、葡萄牙、巴西、塞尔维亚各1篇。国内各省、自治区、直辖市中,第一作者单位为北京的共计180篇,占全部文献的12.6%,具体见表2。
表 2 2010—2020年社区慢性病研究型论文发表地域分布(前10地区)地区 文献数量(篇) 占比(%) 北京 180 12.6 上海 141 9.9 广东 141 9.9 浙江 129 9.0 江苏 127 8.9 湖北 72 5.0 山东 54 3.8 四川 45 3.2 重庆 36 2.5 福建 35 2.5 2.3 社区慢性病管理研究型论文发表机构及来源期刊
发表论文数≥10篇的机构共15家,其中,以华中科技大学发文数量第一,共计36篇,具体见表3。1 427篇文献涉及期刊436种,其中,发文数量≥5篇的期刊73种,发文数量排名前10的期刊详见表4。
表 3 2010—2020年社区慢性病研究型论文发表机构(≥10篇)机构名称 文献数量(篇) 华中科技大学 36 复旦大学 24 北京大学 16 南方医科大学 15 郑州大学 15 中南大学 14 北京协和医学院 14 山东大学 13 南京医科大学 13 杭州师范大学 13 安徽医科大学 12 首都医科大学 12 东南大学 12 上海交通大学 12 天津医科大学 10 表 4 2010—2020年社区慢性病研究型论文来源期刊(前10期刊)期刊名称 文献数量 综合影响因子① 中国全科医学 70 1.601 中国社区医师 47 0.131 中国初级卫生保健 44 0.336 世界最新医学信息文摘 34 — 中国卫生产业 29 0.143 中国慢性病预防与控制 25 1.229 社区医学杂志 24 0.196 临床医药文献电子杂志 23 — 大家健康(学术版) 21 — 中国医药指南 18 0.113 注:“①”表示数据来源于中国知网;“—”表示中国知网未提供相关数据。 2.4 社区慢性病管理研究型论文受基金资助情况
纳入的1 427篇文献中,349篇受相关基金资助,占文献总数的24.5%。其中,国家级基金资助61篇,省部级基金资助114篇,以广东省、上海市最多,分别为15篇和14篇,占省部级基金资助论文的25.4%。
2.5 社区慢性病管理研究型论文高频主题词
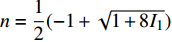
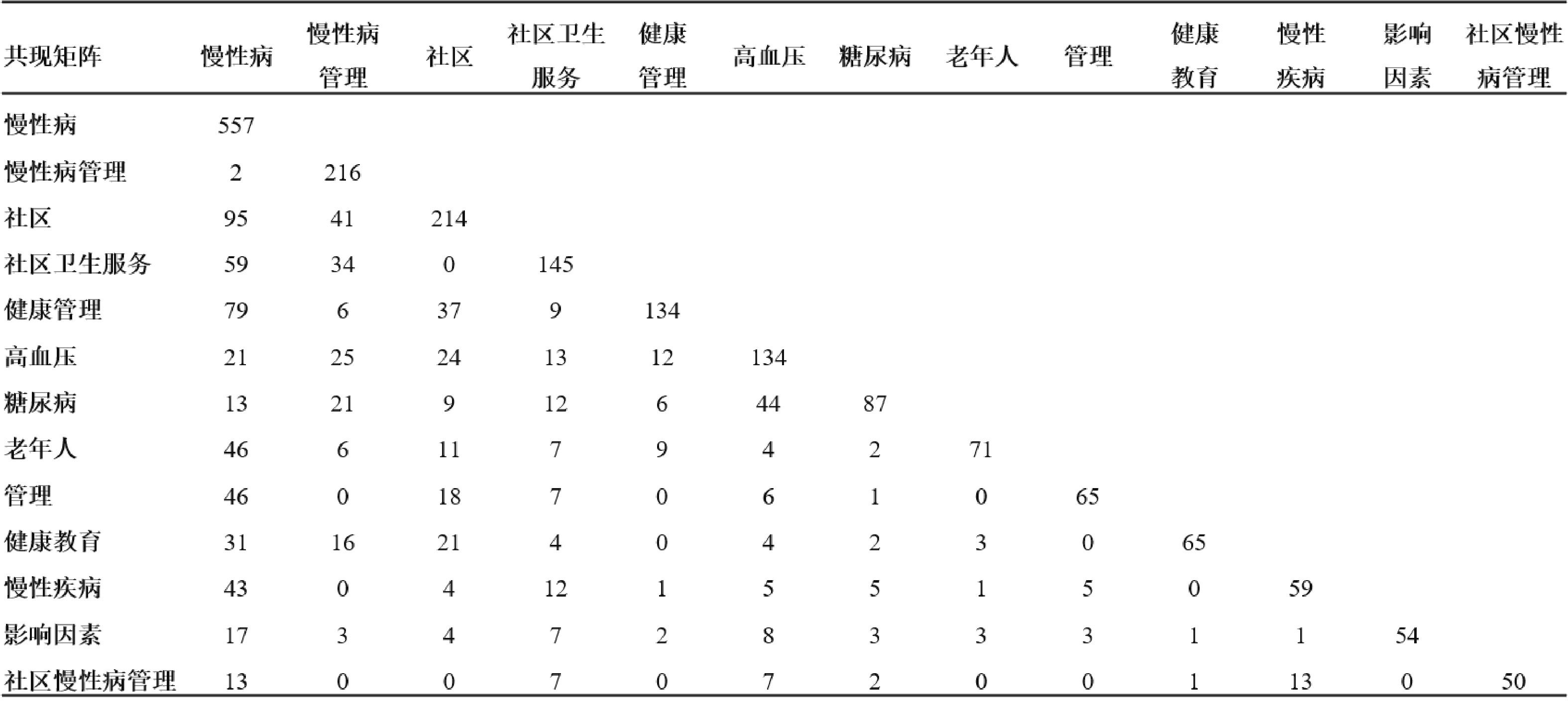
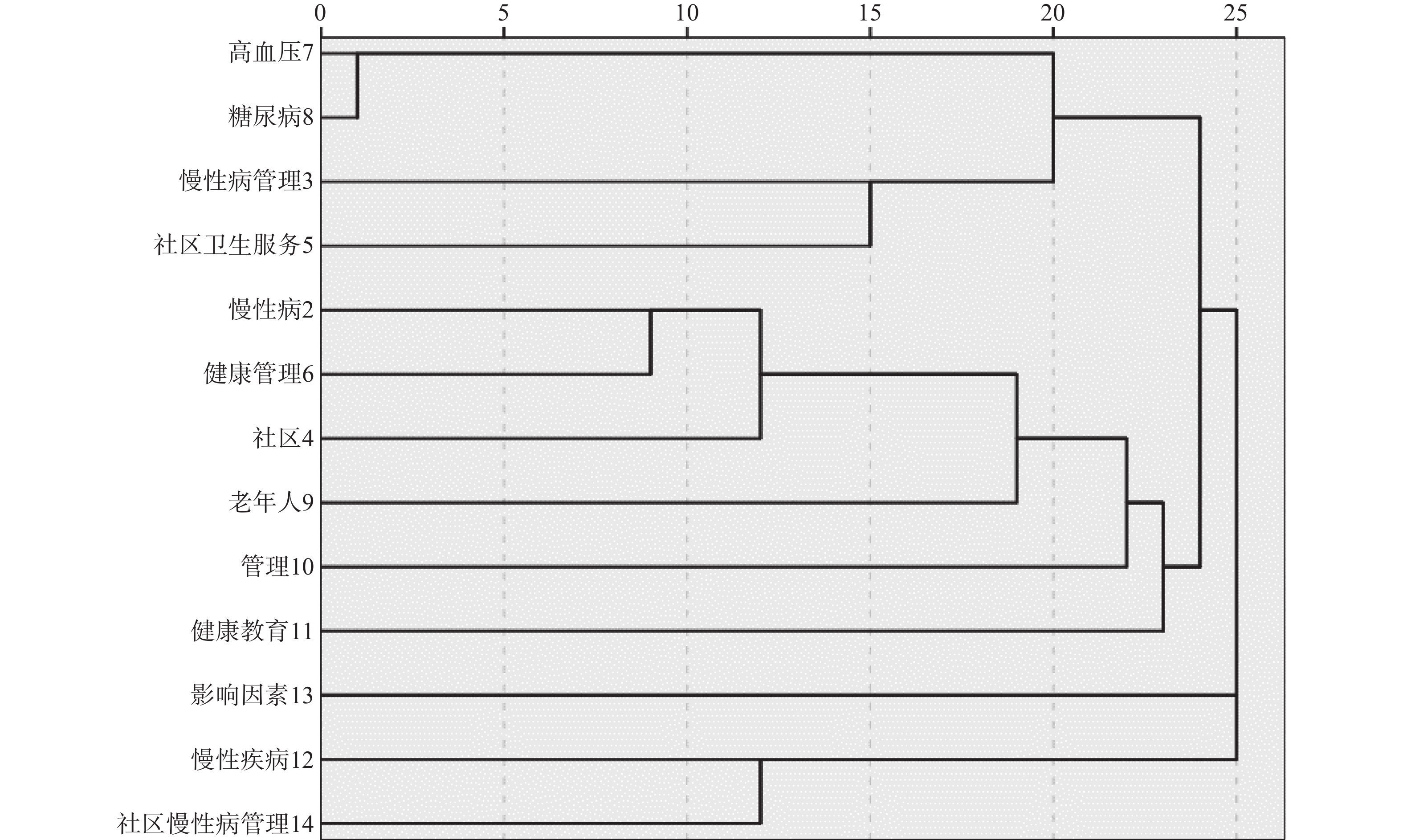
本文以齐普夫第二定律和Donohue据此提出的高频词与低频词临界值分界计算公式为依据,对纳入的1 427篇文献中的关键词进行统计分析,以明确2010—2020年社区慢性病管理研究的热点问题[7-8]。纳入文献共涉及关键词1 769个,其中词频为1的关键词1 279个(I1),根据Donohue公式
$ n=\dfrac{1}{2}(-1+\sqrt{1+8{I}_{1}}) $ ,计算得n=50,即词频≥50的,为本次统计的高频关键词,详见表5。通过Bicomb2.0软件形成词篇和共现矩阵,并在矩阵基础上,应用SPSS 18进行研究主题的聚类分析,见图1、图2。表 5 2010—2020年社区慢性病管理研究型论文高频关键词关键词 出现频次 百分比(%) 累计百分比(%) 慢性病 557 10.03 10.03 慢性病管理 216 3.89 13.92 社区 214 3.85 17.77 社区卫生服务 145 2.61 20.38 健康管理 134 2.41 22.79 高血压 134 2.41 25.20 糖尿病 87 1.57 26.77 老年人 71 1.28 28.05 管理 65 1.17 29.22 健康教育 65 1.17 30.39 慢性疾病 59 1.06 31.45 影响因素 54 0.97 32.42 社区慢性病管理 50 0.90 33.32 3. 讨论
笔者利用Bicomb2.0及SPSS 18对近10年发表于中国学术期刊网络出版总库的社区慢性病管理研究文献进行客观分析,目的在于了解当下热点与难点,为我国社区慢性病管理研究和防治工作推广提供科学依据。
3.1 社区慢性病管理研究现状
本文分析结果显示,2010—2019年社区慢性病管理研究论文的发表数量呈逐年上升的趋势,特别是近3年,论文数量明显增加,2017—2019年共发表相关论文620篇,占全部论文的43.4%。表明有关社区慢性病管理研究在近几年得到重视且发展迅速,这可能与慢性病患者数量增加、经济发展进步导致对社区公共卫生投入的增加,以及患者更关注生活质量等原因有关。
从发表论文的地域分布来看,我国大多数省、市、自治区均有发表,但50.3%的论文分布于北京、上海、广东、浙江、江苏5省份,其中,北京发表的相关研究最多,占全部文献的12.6%;可能与上述5省份经济发达、科研实力强、相关政策支持力度大有关,也与首都北京作为政策起始制定地有关,同时也证明经济较发达的省份相对更加重视社区在慢性病管理中的作用。
从社区相关慢性病管理论文的产出机构及其性质可以看出,发文数≥10篇的研究机构集中于高等院校,是当前社区慢性病管理研究的主力,为我国社区慢性病管理研究提供了科学理论依据,原因可能为高等院校研究氛围浓郁、研究条件优良及研究人力资源充足等。
从来源期刊的数据分析来看,文章发表数量前10的期刊以《中国全科医学》杂志发文最多,说明上述期刊为当前我国社区的慢性病管理研究的主要交流载体和平台;同时通过期刊影响因子分析,仅《中国全科医学》综合影响因子>1,其余均<1或缺少影响因子,表明当前社区慢性病管理研究虽然受到越来越多研究者的重视,但研究水平较低,论文质量不高,这可能与该类研究集中于基层医院且样本量较少有关,同时也反映出该类研究具有巨大的提升潜力,值得更多关注。
由于基金论文学术价值较高,且可以反映某一研究领域内的前沿问题和研究动态,因此,本次文献分析也针对论文的基金资助情况进行分析。结果显示,24.5%的论文受到基金资助,其中国家级、省部级及其他基金占总资助的比例分别为17.5%、32.7%及49.9%,且受资助的城市中,以广东省、上海市最多,表明目前在社区相关的慢性病管理领域主要依赖其他基金资助,同时发达省市获资助比例最大,可能与我国社会主义初级阶段国情以及社区公共卫生服务还处于基础阶段、慢性病管理研究近年来逐渐起步等原因有关。
3.2 社区慢性病管理研究热点
通过共现矩阵和聚类分析研究本次文献的高频关键词后发现,社区的慢性病管理研究热点主要集中在对慢性病进行健康管理、针对慢性病的社区卫生服务、对糖尿病/高血压开展慢性病管理、面向老年人的健康教育以及影响因素分析等方面。可能与糖尿病、高血压患病人群基数较大、该类疾病主要群体为老年人,缺乏一定自我管理能力等因素有关。同时根据关键词分析,显示关于我国社区慢性病管理的研究尚未成熟,未形成较为成熟的管理体系,多数研究均属于探索阶段。
对于以上问题,笔者认为与我国政策和经费缺乏两大难题有关[9],首先是我国医疗资源分配不均衡,社区卫生服务长期人员配备不足,医疗康复设备不完善,难以发挥有效的慢性病管理防治作用,导致需要慢性病管理服务的社区居民流向大型医院,加剧资源分配不均的现象。其次,关于社区慢性病防治研究的理论实践并未成熟,难以实现理想的控制效果,因此还有待于我国学者继续努力。
3.3 未来相关研究的启示
本文的文献计量学分析结果显示,我国社区慢性病管理研究在近年来受到各方越来越多的关注,且已经取得一定成果。例如,北京、上海、广州等发达城市先后开展社区慢性病综合管理研究,且受到各方基金的资助,高校作为理论研究的主力发挥重要作用,同时大多数研究立足于我国国情,对患病人数较多的糖尿病、高血压老年患者开展健康教育、社区卫生服务。另外,通过大量的文献研究,国内研究者已逐渐认识到社区在慢性病防治工作中的重要作用,但由于大多数研究存在样本量较少等原因,该类研究仍处于起步阶段。
因此,在延续前人成果的基础上,首要策略是增加对社区慢性病防治工作的投入,利用国家政策保证社区充分发挥慢性病防治工作的能动性,同时还可通过动员其他资金,如引进私企或外资减轻地方财政负担,并在社区建立慢性病医疗补助专项资金。其次,可在医药卫生制度改革时考虑增加社区慢性病防治工作的医疗人员,保证当地居民的医疗、保健需求。最后,还可利用互联网技术,建立社区互联网互助系统,定期更新慢性病自我管理的相关科学知识,通过医疗工作者与患者、患者之间的灵活沟通,实现慢性病防治的目的。
4. 小结
通过对2010年1月至2020年1月期间我国社区慢性病管理相关研究论文的分析,本研究得到以下结论:①社区慢性病管理的研究呈逐年上升趋势,研究地域主要集中在经济发达地区,高校为主要研究机构,但相关研究论文质量和学术水平较低,受国家资金资助较少。②社区慢性病管理研究热点集中且局限,尚未形成成熟的理论体系。但本文同样具有一定局限性,首先,主要集中在中国学术期刊网络出版总库发表的学术文献,范围较小且中文论文较多,其次,分析软件也有局限性,如Bicomb2.0只能分析已发表的文献[10]。笔者将进一步加大相关领域研究的广度和深度,为我国社区慢性病管理提供理论参考依据。
-
表 1 4组患者基本资料比较[n(%),
$\bar x$ ±s]组别 年龄(岁) 男性 BMI(kg/m2) 收缩压
(mmHg)舒张压
(mmHg)TC
(mmol/L)TG
(mmol/L)HDL-C
(mmol/L)LDL-C
(mmol/L)单纯水化组(n=50) 60.58±11.35 28(56) 23.96±2.91 130.62±16.99 79.98±13.04 4.48±0.91 1.43±0.84 1.26±0.34 2.55±0.71 β-受体阻滞剂组(n=47) 64.40±11.61 32(68) 25.13±3.60 125.79±15.93 74.89±13.19 4.03±0.99 1.50±0.91 1.09±0.35 2.30±082 ACEI/ARB组(n=50) 65.04±6.52 25(50) 24.37±3.05 134.86±17.17 76.52±10.29 4.15±0.97 1.60±0.91 1.16±0.30 2.28±0.80 CCB组(n=46) 65.67±9.25 26(57) 24.45±2.81 139.43±14.57 78.91±9.28 4.23±0.87 1.34±0.61 1.20±0.30 2.38±0.74 组别 UA(μmol/L) FBG
(mmol/L)造影剂用量(ml) Scr
(μmol/L)BUN
(mmol/L)eGFR[ml/
(min·1.73 m2)]eGFR>90 [ml/
(min·1.73 m2)]eGFR<60 [ml/
(min·1.73 m2)]Ccr
(ml/min)单纯水化组(n=50) 330.48±82.36 5.35±1.06 122.32±56.11 63.62±16.01 5.25±1.17 112.04±27.17 11(22) 1(2) 97.86±29.83 β-受体阻滞剂组(n=47) 378.19±87.31 5.32±1.87 124.83±60.38 66.30±14.61 5.32±1.48 107.05±19.59 8(17) 1(2) 95.88±26.84 CEI/ARB组(n=50) 363.88±98.07 5.50±1.25 121.79±59.22 64.94±12.69 5.48±1.30 103.26±20.23 12(24) 1(2) 89.91±23.94 CCB组(n=46) 343.87±81.79 5.40±1.58 126.48±58.76 63.57±13.90 5.51±1.34 106.93±20.12 8(17) 1(2) 91.98±28.75 表 2 4组患者造影前后肾功能指标的比较
组别 Scr(μmol/L) BUN(mmol/L) eGFR[ml/(min·1.73 m2)] Ccr(ml/min) 术前 术后48 h 术前 术后48 h 术前 术后48 h 术前 术后48 h 单纯水化组(n=50) 63.62±16.01 64.04±16.66 5.25±1.17 5.34±1.33 112.04±27.17 110.27±25.58 97.86±29.83 97.42±30.39 β受体阻滞剂组(n=47) 66.30±14.61 64.53±14.00 5.32±1.48 4.71±1.01*▲ 107.05±19.59 105.61±18.35▲ 95.88±26.84 98.88±28.55 ACEI/ARB组(n=50) 64.94±12.69 64.98±13.28 5.48±1.30 5.26±1.47 103.26±20.23 103.23±20.29 89.91±23.94 90.02±24.70 CCB组(n=46) 63.57±13.90 63.28±13.27 5.51±1.34 5.42±1.30# 106.93±20.12 111.52±24.62 91.98±28.75 92.20±30.06 *P<0.05,与单纯水化组比较;#P<0.05,与β受体阻滞剂组比较;▲P<0.05,与同组术前比较。 表 3 β受体阻滞剂组不同血压水平造影前后肾功能指标的比较
肾功能指标 SBP<140且DBP<90(n=34) SBP≥140或DBP≥90(n=13) 术前 术后48 h 术前 术后48 h Scr(μmol/L) 64.85±11.72 63.28±11.79 70.08±20.49* 67.81±18.78 BUN(mmol/L) 5.31±1.59 4.71±1.05 5.36±1.19 4.71±0.92 eGFR(ml/(min·1.73 m2) 108.58±18.10 105.40±20.44 103.06±23.38 107.77±12.16 Ccr(ml/min) 95.55±23.13 98.53±25.74 96.74±35.91* 99.75±36.06 *P<0.05,与SBP<140且DBP<90组比较。 -
[1] MAWRI S, MICHAELS A, GIBBS J, et al. CRT-100.78 ACE inhibitors and ARBs in post-percutaneous coronary intervention contrast-induced nephropathy (CIN): to hold or not to hold? JACC: Cardiovasc Interv,2018,11(4):S22. [2] VACHHARAJANI T, HOSSAIN M, COSTANZO E, et al. Contrast-Induced nephropathy: Pathophysiology, risk factors, and prevention[J]. Saudi J Kidney Dis Transpl,2018,29(1):1. doi: 10.4103/1319-2442.225199 [3] KODZWA R. ACR manual on contrast media: 2018 updates[J]. Radiol Technol,2019,91(1):97-100. [4] JO S H, LEE J M, PARK J, et al. The impact of renin-angiotensin-aldosterone system blockade on contrast-induced nephropathy: a meta-analysis of 12 studies with 4, 493 patients[J]. Cardiology,2015,130(1):4-14. doi: 10.1159/000366473 [5] CHEN Y T, CHAN C K, LI W Y, et al. Renin-angiotensin-aldosterone system inhibition decreased contrast-associated acute kidney injury in chronic kidney disease patients[J]. J Formos Med Assoc,2021,120(1):641-650. doi: 10.1016/j.jfma.2020.07.022 [6] WOLAK T, ALIEV E, ROGACHEV B, et al. Renal safety and angiotensin II blockade medications in patients undergoing non-emergent coronary angiography: a randomized controlled study[J]. Isr Med Assoc J,2013,15(11):682-687. [7] ROSENSTOCK J L, BRUNO R, KIM J K, et al. The effect of withdrawal of ACE inhibitors or angiotensin receptor blockers prior to coronary angiography on the incidence of contrast-induced nephropathy[J]. Int Urol Nephrol,2008,40(3):749-755. doi: 10.1007/s11255-008-9368-1 [8] ROSADO INGELMO A, DOÑA DIAZ I, CABAÑAS MORENO R, et al. Clinical practice guidelines for diagnosis and management of hypersensitivity reactions to contrast media[J]. J Investig Allergol Clin Immunol,2016,26(3):144-155; quiz2pfollowing155. doi: 10.18176/jiaci.0058 [9] 李飞, 杨定平. 对比剂肾病的发病机制及防治[J]. 临床肾脏病杂志, 2013, 13(9):426-429. [10] 陈彩玲, 黄铮, 赖雯苑, 等. ACEI/ARB与CCB防治高血压病伴慢性肾功能不全患者发生造影剂肾病的效果比较[J]. 心脏杂志, 2015, 27(6):703-707. [11] OGUZHAN N, CILAN H, SIPAHIOGLU M, et al. The lack of benefit of a combination of an angiotensin receptor blocker and calcium channel blocker on contrast-induced nephropathy in patients with chronic kidney disease[J]. Ren Fail,2013,35(4):434-439. doi: 10.3109/0886022X.2013.766566 [12] 王仁秀, 姜松, 解秀芬, 等. 经皮冠状动脉介入治疗后并发造影剂肾病危险因素的Meta分析[J]. 实用心脑肺血管病杂志, 2020, 28(9):74-80. doi: 10.3969/j.issn.1008-5971.2020.09.015 [13] MOLEN A J, REIMER P, DEKKERS I A, et al. Post-contrast acute kidney injury - Part 1: Definition, clinical features, incidence, role of contrast medium and risk factors[J]. Eur Radiol,2018,28(7):2845-2855. doi: 10.1007/s00330-017-5246-5 [14] 王琼涛, 吉六舟, 张进锋, 等. 冠心病患者经皮冠状动脉介入术后发生造影剂肾病的危险因素[J]. 中华实用诊断与治疗杂志, 2019, 33(11):1078-1081. [15] WANG M, ZHANG L, YUE R Z, et al. Significance of cystatin C for early diagnosis of contrast-induced nephropathy in patients undergoing coronary angiography[J]. Med Sci Monit,2016,22:2956-2961. doi: 10.12659/MSM.897241 [16] DAVENPORT M S, PERAZELLA M A, YEE J, et al. Use of intravenous iodinated contrast media in patients with kidney disease: consensus statements from the American college of radiology and the national kidney foundation[J]. Kidney Med,2020,2(1):85-93. doi: 10.1016/j.xkme.2020.01.001 期刊类型引用(1)
1. 张月婷,李新春,关玲霞,冯世军. 三七皂苷对动脉损伤后血管内膜炎症、应激和增生的影响. 中华实验外科杂志. 2023(07): 1347-1350 .  百度学术
百度学术其他类型引用(0)
-





 下载:
下载:

 下载:
下载: 


